Recognizing Sarcoidosis: Get the facts
Click the image below to check out our interactive tool, Recognizing Sarcoidosis
Sarcoidosis Symptoms
ABOUT SARCOIDOSIS
SYMPTOMS
Most people who have sarcoidosis have no signs or symptoms of the disease. In these cases, it is diagnosed when a chest x-ray is done for another reason, and it is found to be abnormal.
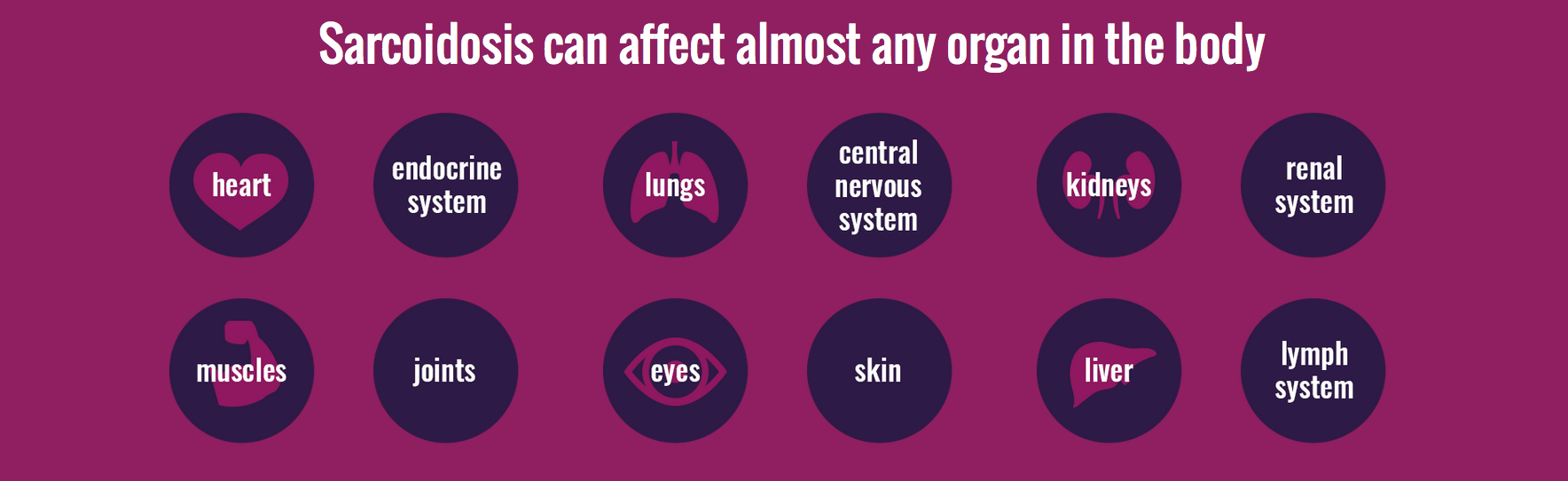
Because sarcoidosis so often affects the lungs, the most common symptoms of sarcoidosis include shortness of breath and chronic cough. Because sarcoidosis can affect the entire body, a wide variety of symptoms can be seen with sarcoidosis. Other symptoms of sarcoidosis include:
- Fatigue
- Shortness of breath
- Unexplained weight loss
- Night sweats
- Overall feeling of sickness
- Swollen lymph nodes
- Irregular heart beat
- Swollen legs
- Headaches
- Visual problems
- Weakness or numbness of an arm, leg, or part of your face
- Painful or red, raised bumps on the legs or arms
- Discoloration of the nose, cheeks, lips, and ears
- Scaly-appearing skin rash
- Joint pain
- Muscle swelling and soreness
- Arthritis
- Burning, itching, tearing, or pain in the eyes
- Red eyes
- Sensitivity to light
- Blurred vision
- Fever
RISK FACTORS
Sarcoidosis can affect people of any age, race, and gender. Mostly, though, the disease strikes adults between the ages of 20 and 30. It is most common in African-Americans and people of Northern European—particularly Scandinavian—descent. The disease is slightly more common in women than in men.
The disease manifests (shows up) differently in different groups of people. While the lungs and lymph nodes are affected in almost everyone who has sarcoidosis, African-Americans and people of Japanese descent are more like to have eye involvement than Caucasians. Skin lumps are most likely to affect people of Northern European descent, and those with a Japanese background.
CAUSES
No one knows exactly what causes sarcoidosis. The fact that someone is more likely to develop the disease if someone in his or her close family has sarcoidosis suggests that genetics plays a role. Researchers haven't yet found a gene or genes linked to the development of sarcoidosis, but they continue to look.
Some research suggests that bacteria, viruses, or chemicals might trigger the disease. Such triggers, although usually harmless in most people, might irritate the immune systems of people who are at genetic risk for developing sarcoidosis. ricans and people of Japanese descent are more like to have eye involvement than Caucasians. Skin lumps are most likely to affect people of Northern European descent, and those with a Japanese background seem prone to sarcoidosis-related heart problems.
COMPLICATIONS
Sarcoidosis can cause serious health problems. It's important to remember, though, that most cases of sarcoidosis are not severe and do not cause lasting damage to the body.
Sarcoidosis of the lungs can lead to the development of scar tissue in the lungs, a condition called pulmonary fibrosis. Pulmonary fibrosis can make it difficult for the lungs to effectively take in air and oxygen. Severe pulmonary fibrosis can lead to respiratory failure and death.
Other sarcoidosis-related lung complications include pulmonary hypertension (high blood pressure in the major arteries leading to the lungs) and mucus buildup in the airways (which makes it difficult to breathe and increases the likelihood of developing lung infections).
Sarcoidosis that affects the eyes can cause inflammation that may lead to glaucoma, cataracts, or blindness. These complications are usually avoided with good medical care and treatment.
Sarcoidosis sometimes affects the heart and can cause irregular heartbeat, heart failure, and heart attacks. Because these problems can lead to severe complications, everyone with sarcoidosis should be screened for cardiac (heart) sarcoidosis. Appropriate treatment can help avoid these complications.
Other complications of sarcoidosis include:
- High blood calcium levels
- Liver disease
- Peripheral neuropathy, a change in the sensitivity of the peripheral nerves (usually those in your hands and feet)
- Meningitis, an inflammation of the tissues surrounding the brain and spinal cord
- Bone and joint damage
- Muscle weakness
- Kidney failure
Remember, though, that MOST people with sarcoidosis do not experience any serious complications.
Back to Top
SARCOIDOSIS TREATMENT
TREATMENT AND DRUGS
In most cases of sarcoidosis, no treatment is necessary. Sarcoidosis may go away without medical treatment.
Medical treatment can be used to control symptoms, prevent complications, and improve outcomes in patients with persistent sarcoidosis. If you have sarcoidosis, your health-care provider will carefully monitor you to see if your sarcoidosis is getting better or worse and will adapt your treatment depending on how your body is doing.
Sarcoidosis is often treated with the help of a multidisciplinary team of health-care professionals. Because the disease can affect so many organ systems, you may work with health-care providers who specialize in the treatment of the lungs, heart, brain, kidneys, liver, eyes, and skin. At specialized medical centers, these health-care providers work as a team to develop a comprehensive treatment plan to control your symptoms and protect your overall health.
Medications used to treat sarcoidosis include:
Corticosteroids. Corticosteroids reduce inflammation. They are not the same as anabolic steroids, the type of steroid that is sometimes abused by athletes. Corticosteroids are the primary treatment for sarcoidosis. Treatment with corticosteroids relieves symptoms in most people within a few months. The most commonly used corticosteroids are prednisone and prednisolone. People with sarcoidosis may need to take corticosteroids for many months. Because these medications can cause side effects (including weight gain, insomnia, mood swings, acne, difficulty regulating blood sugar, and bone loss), your health-care provider will gradually decrease your dose of medication after you start to take it. The goal is to stabilize symptoms without unnecessary exposure to more corticosteroids than you need to control the disease.
Immune system suppressant medication. Because sarcoidosis may be the result of an overreaction of the immune system, suppressing the immune system may ease symptoms and prevent further organ damage. When corticosteroids are not effective, your provider may talk with you about starting other medications, including methotrexate, azathioprine, and mycophenolate mofetil. Other medications may help a few patients who do not respond to other therapies. They may include cyclophosphamide and biologics response modifiers (biologics or TNF-blockers).
Antimalarial drugs. These medications were originally used (and are still used) to treat malaria. As a treatment for sarcoidosis, these drugs are most likely to be effective in people who have musculoskeletal symptoms, skin disease or a high level of calcium in their blood. Hydroxychloroquine and chloroquine are antimalarial drugs that are used to treat sarcoidosis. Both can cause stomach irritation and eye problems.
People with severe or advanced lung sarcoidosis may need oxygen therapy. In a few cases lung transplantation—the replacement of a diseased lung or lungs with a healthy donor lung—is used to treat severe lung sarcoidosis.
PREPARE FOR YOUR APPOINTMENT
Because sarcoidosis usually involves the lungs, it may not be that difficult to diagnose with a chest x-ray. However, it might be more difficult because it may not involve the lungs and may have a wide variety of symptoms. You can help your health-care provider by compiling a list of your symptoms, including when they appeared and what, if anything, makes them worse or better.
Your health-care provider will want to know as much as possible about your overall health and medical history, so bring the following information to your appointment:
- A complete list of your medications, supplements, and vitamins. Include all prescription and over-the-counter medications and supplements, even herbal and natural remedies. If possible, bring the bottles and containers with you to your appointment so your health-care provider can see exactly what you're taking.
- Your medical history. If you have medical records at another clinician's office, ask to have copies sent to your current health-care provider.
- Family history. Has anyone in your family ever been diagnosed with sarcoidosis or had symptoms of sarcoidosis? Is there a history of other lung, skin, or heart problems?
- Questions. Write down any questions you may have, so you don't forget to ask them when you're at your appointment.
LIFESTYLE AND HOME REMEDIES
Staying as healthy as possible increases your odds of living a full, satisfying life with sarcoidosis. A well-balanced diet (high in vegetables, fruits, whole grains, and low-fat proteins) provides your body with the nutrients it needs to stay healthy. Regular exercise keeps you fit and improves your body’s ability to efficiently use oxygen. Adequate rest decreases stress and increases feelings of well-being.
If you smoke, quit. Smoking causes additional damage to the lungs. It’s not easy to stop smoking, but your health-care provider can help. He or she can prescribe medication to help you stop smoking and can also refer you to local classes and support groups that will help you stop smoking.
See your health-care provider for regular appointments. It’s also important to schedule routine eye exams. Sarcoidosis—and some medications used to treat sarcoidosis—can affect and damage the eyes. Regular eye exams help detect eye changes so that steps can be taken to preserve eye health and vision. Ask your health-care provider how often you have should have your eyes professionally examined.
Back to Top
SARCOIDOSIS DIAGNOSIS
TESTS AND DIAGNOSIS
 Your health-care provider will take your medical history and perform a physical examination. Medical tests provide additional information. Because many of the symptoms that occur with sarcoidosis also occur with other diseases, your health-care provider may work to rule out those diseases.
Your health-care provider will take your medical history and perform a physical examination. Medical tests provide additional information. Because many of the symptoms that occur with sarcoidosis also occur with other diseases, your health-care provider may work to rule out those diseases.
Test commonly used to look for sarcoidosis include:
- Chest x-ray. A chest x-ray is a painless test that allows your clinician to look at your lungs and airways. Although more than 90% of people with sarcoidosis will have abnormal x-rays, many other conditions can cause abnormal x-rays too. Often, a clinician will notice signs of sarcoidosis on an x-ray that was ordered for other purposes.
- CT scans. A CT scan (sometimes called a "CAT scan") uses x-rays to create cross-sectional pictures of the body. During a CT scan, the patient lies on a narrow table that can slide in and out of a tube-shaped scanner. It's important to stay still during the exam, so the machine can take clear pictures. Because your muscles, bones, and lungs move with every breath, you may be asked to hold your breath for brief periods. Some CT scans require the use of contrast, a special dye that helps certain things show up more clearly on the resulting pictures. The contrast is given through an IV. If your exam requires the use of contrast, a health-care provider will let you know.
- Lung function tests (also called pulmonary function tests or PFTs). Your health-care provider may have you breathe out into a mouthpiece that's attached to a spirometer, a device that measures the amount and speed of air you blow out. This test gives information about how well your lungs are working. Other equally painless tests may be prescribed. Lungs affected by sarcoidosis generally don't work as well as healthy lungs.
- Lung biopsy. If your chest x-ray, CT scan, lung function tests, and symptoms suggest sarcoid involvement in the lungs or lymph nodes around the lungs, your health-care provider may obtain samples of lung tissue or lymph nodes tissue. The tissue can be analyzed in a laboratory to see if it shows signs of sarcoidosis. Pulmonary specialists can obtain lung tissue samples with bronchoscopy. This procedure is usually done in a hospital, but does not require admission. A bronchoscope is a thin, flexible tube that is placed into your airways and lungs through your nose or mouth. Specimens are obtained through this tube. Medication will be used to numb your throat before the procedure, and you will be given medication to sedate you for the procedure.
- Other biopsies. If you have bumps or lesions on your skin that may be related to sarcoidosis, your health-care provider may take tissue samples and send them to the lab for analysis.
- Blood tests. Many people with sarcoidosis make excess amounts of a chemical called angiotensin-converting enzyme. Blood tests can be used to detect high levels of this substance. However, other conditions also cause elevated level vitamin D and angiotensin-converting enzymes, so these tests can't be used to confirm a sarcoidosis diagnosis. Blood tests can also be used to check white and red blood cell levels and to look for evidence of liver or kidney damage.
 MRI (magnetic resonance imaging). Like x-rays and CT scans, MRI tests provide a glimpse inside the body. MRIs can be used to look for signs of sarcoidosis in the brain, spinal cord, heart, bones, and other organs.
MRI (magnetic resonance imaging). Like x-rays and CT scans, MRI tests provide a glimpse inside the body. MRIs can be used to look for signs of sarcoidosis in the brain, spinal cord, heart, bones, and other organs.- Nuclear imaging. These tests use radioactive dye to help clinicians see blood flow through various body organs. The dye is injected into your veins before the scan. After a period of time, your body is scanned with a special camera that can detect the radiation from the dye. Nuclear imaging tests are sometimes used to help diagnose sarcoidosis of the heart.
- Positive emission tomography (PET scan). This imaging test also uses a radioactive substance to provide information about an organ's functioning. PET scans are often used to help diagnose cardiac sarcoidosis or to find a good spot to biopsy.
- Heart rhythm monitoring. Your health-care provider may use electrocardiography (often called ECG or EKG) to get information about the functioning of your heart. Up to 50% of people with sarcoidosis will have an abnormal EKG, so additional testing might be needed to see whether the changes are worrisome.
- Echocardiogram. An echocardiogram is an ultrasound of the heart. It uses ultrasound waves to look at the heart. (Pregnancy ultrasounds use the same technology to provide a look at the fetus.) Your health-care provider might order an echocardiogram to see how the heart is pumping blood.
Back to Top
RESOURCES
Sharable Digital Tools
Click any image below to download and share on Twitter, Facebook, or LinkedIn.
Cover Images
Facebook
Twitter
LinkedIn
Profile Images
Facebook
Twitter
LinkedIn
Social media postcards
Facebook and Twitter
LinkedIn
PDFs
Click the links below to download as PDFs.
Sarcoidosis Patient Toolkit
Sarcoidosis Clinician Toolkit
Sarcoidosis Proclamation
Additional Websites
American Lung Association Website
American Lung Association Webinar
American Lung Association Better Breathers Clubs
FSR Inspire Online Support Community
Patient Stories
Calendar of Events
FSR Patient Registry
FSR Physician Directory
CHEST Education for RTs and RNs
Back to Top
UNDERSTANDING SARCOIDOSIS: SOURCES
1 Foundation for Sarcoidosis Research website: stopsarcoidosis.org/patient-resources/what-is-sarcoidosis
2 Foundation for Sarcoidosis Research infographic: pinterest.com/pin/477522366711934075
3 Nunes H, Bouvry D, Soler P. Sarcoidosis. Orphanet Journal of Rare Diseases. 2007; 2(46)
Patient education resources supported in part by grants from Mallinckrodt Pharmaceuticals.