Hot Topics in CHEST November 2020
By: Chris Carroll, MD, FCCP
November 9, 2020
 Each month, we ask our Social Media Co-Editors of CHEST to weigh in on the hot topics in CHEST. It's November, so let's hear from one of our co-editors, Dr. Chris Carroll, as he outlines his highlights. After reviewing the issue, be sure to share your hot list on Facebook, tweet with the hashtag #journalCHEST, or discuss in the CHEST LinkedIn group.
Each month, we ask our Social Media Co-Editors of CHEST to weigh in on the hot topics in CHEST. It's November, so let's hear from one of our co-editors, Dr. Chris Carroll, as he outlines his highlights. After reviewing the issue, be sure to share your hot list on Facebook, tweet with the hashtag #journalCHEST, or discuss in the CHEST LinkedIn group.
How excited I am to be guest hosting the November Hot in CHEST blog! Can it really be November already? Does time have any meaning anymore? Well, at least there is a new issue of the journal CHEST® to distract us! So let’s dive into it!
Recently, there has been increased focus on the consequences of the therapies we provide in the intensive care unit. Although life-saving, these therapies often can be associated with significant long-term morbidities and can continue to burden patients for years after ICU discharge.
One of these under-recognized adverse events of critical illness is dysphagia following extubation. In this issue of the journal, there are two articles by Zuercher and colleagues as well as Moss and colleagues that provide support for techniques that allow for early identification of dysphagia.
A study by Zeurcher examined 933 patients following extubation to identify risk factors of developing post-extubation dysphagia. The authors used a simple water swallow screening tool to identify patients at risk within 3 hours of extubation. The water swallow test consists of swallowing 3 teaspoons of water and then drinking one-half a glass of water. Failure in two screenings triggered an examination by a dysphagia specialist. The authors found that 12% of patients screened positive for dysphagia and that duration of invasive mechanical ventilation, baseline neurological disease, and emergency admission were independent risk factors for post-extubation dysphagia. Widespread implementation of this simple tool would allow for more rapid identification of dysphagia in this population.
And a study by Moss also evaluated patients for dysphagia following extubation. A cohort of 213 patients underwent a more formal bedside swallowing evaluation by speech and language pathologists. Patients also underwent a flexible endoscopic evaluation of swallowing to look for direct aspiration. One-third of these patients had aspiration by endoscopy, 52% of which were detected by bedside swallowing evaluation. The authors used these results to develop a decision tree algorithm that had high sensitivity and accuracy for aspiration.
Taken together, these studies provide an important step in the identification of this under-recognized complication of critical illness.
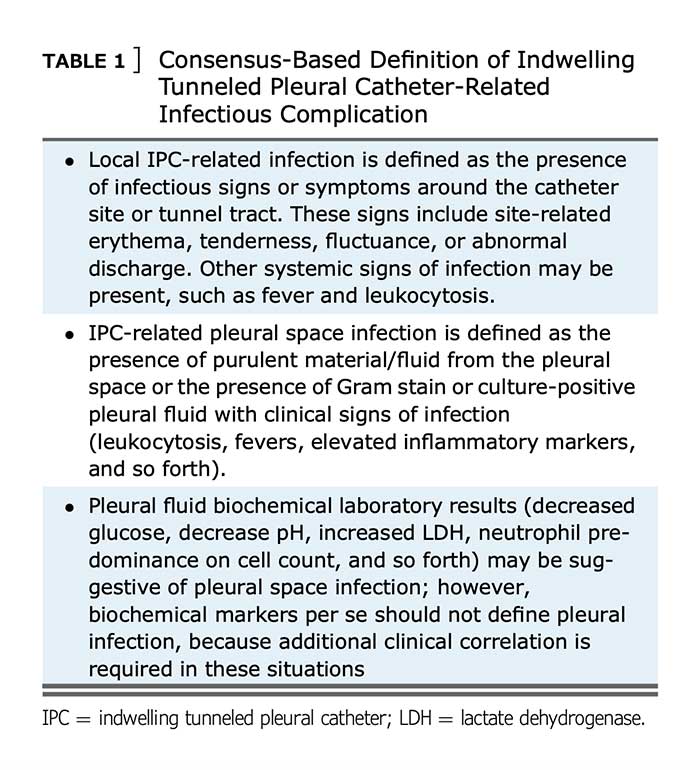
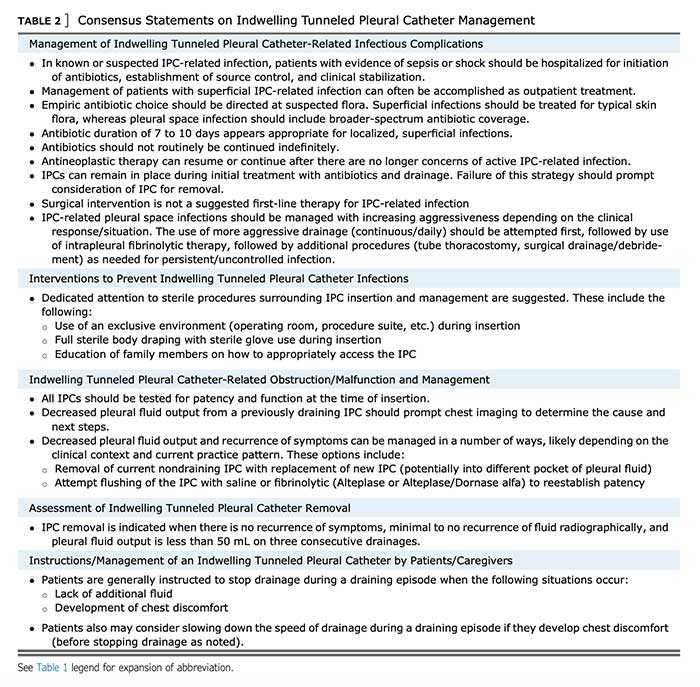
Also in this month’s journal issue, there is an important consensus statement on the management of indwelling tunneled pleural catheters (IPC). These catheters are frequently used in the management of recurrent pleural effusions, and with the increased usage, there is a need for consensus statements in order to attempt to reduce complications and direct further research. This group used a modified Delphi approach to develop statements related to perioperative and long-term IPC management.
A strong consensus was achieved on defining indwelling tunneled pleural catheter-related infectious complications, management of these complications, interventions to prevent infections, management of obstruction and malfunction, removal, and instructions for patients/caregivers. Check out the full paper for details!
And finally, Chaudhuri and colleagues have conducted a systematic review and meta-analysis of the use of high-flow nasal cannula (HFNC) in the immediate postoperative period. HFNC has been increasingly used in the prehospital, hospital, and ICU setting and has been shown to reduce intubation in acute hypoxic respiratory failure. In this review, Chaudhuri evaluates 11 randomized clinical trials (including 2201 patients), comparing HFNC use to conventional oxygen therapy and noninvasive positive pressure in the postoperative period. The authors found that HFNC was associated with a lower reintubation rate and decreased escalation of respiratory support when compared with conventional oxygen therapy. Additionally, a post hoc subgroup analysis found that this effect was largely due to patients who were obese and/or high-risk following cardiac surgery.
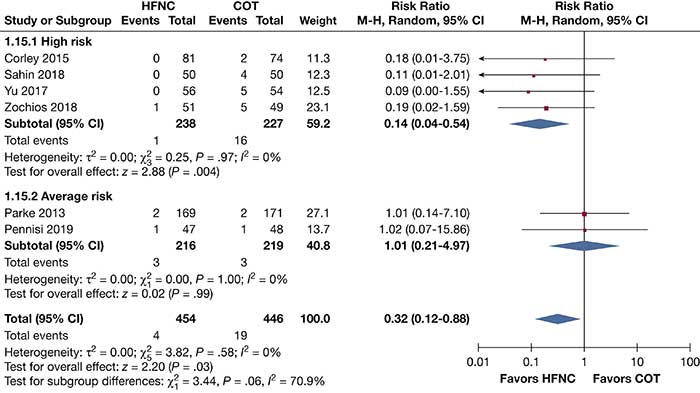
All too often we provide therapies in the ICU without proven benefit. However, this study provides some evidence that prophylactic HFNC may be beneficial in a subgroup of postoperative patients.