Hot in Journal CHEST: June 2021
By: Vineesha Arelli, MD
June 4, 2021
Hello fellow CHEST members and friends of the pulmonary and critical care medicine world. As summer officially begins, I feel that there has been a collective sigh of relief as, hopefully (at least in parts of the US and as repeatedly stated by my 6-year-old son), “COVID is ending.” Though the journey has been unique for each of us, we have all traveled it together. I hope each of you is having a chance to reboot. As a community physician serving the middle Tennessee area, I have had the opportunity to engage in the challenges of rural medicine. I have also witnessed how up-to-date scientific guidelines from large medical associations, such as CHEST, were critical and swiftly used during the pandemic. Science has prevailed and my patients are slowly warming back up to recommendations from major medical institutions. Before diving into this month’s review of What’s Hot in CHEST®, I would like to thank my fellow Social Media Co-Editor, Dr. Divya Patel, for her warm welcome in last month’s blog.
In the past year, the COVID-19 pandemic has brought national attention to disparities in respiratory morbidity and mortality. Since 1950, non-Hispanic blacks (NHBs) have experienced higher rates of mortality than non-Hispanic whites (NHWs). In a study in CHEST, Donaldson and colleagues hypothesized that geographic variation existed in the magnitude of black-white racial disparities in mortality rates from influenza and pneumonia. Using data from 1999 to 2018, age-adjusted mortality rates (AAMRs) were computed by race for Health & Human Services (HHS) regions. The authors found that AAMRs were higher in NHBs than NHWs in each age group and in seven of 10 HHS regions. The disparity in influenza and pneumonia mortality rates were greatest in HHS regions 2 (New York and New Jersey) and 9 (California, Arizona, Hawaii, and 19 delta counties in Nevada). Within these regions, disparities were greatest in the core of major metropolitan areas. There was a nearly threefold difference between the highest and lowest rates observed. The authors concluded that further research is needed to inform targeting resources to reduce these disparities.
Clinical studies have shown that dexmedetomidine improves noninvasive ventilation (NIV) comfort in patients with acute respiratory failure. Lewis and colleagues wanted to answer if dexmedetomidine, when compared with another sedative or placebo, reduces the risk of delirium, mortality, need for intubation and mechanical ventilation, or ICU length of stay (LOS) in adults with acute respiratory failure initiated on NIV in the ICU. They electronically searched MEDLINE, EMBASE, and the Cochrane Library for randomized controlled trials (RCTs). Analysis of 12 RCTs showed that use of dexmedetomidine reduced the risk of intubation, delirium, and ICU LOS. The downside was that dexmedetomidine was associated with an increased risk of bradycardia and hypotension.
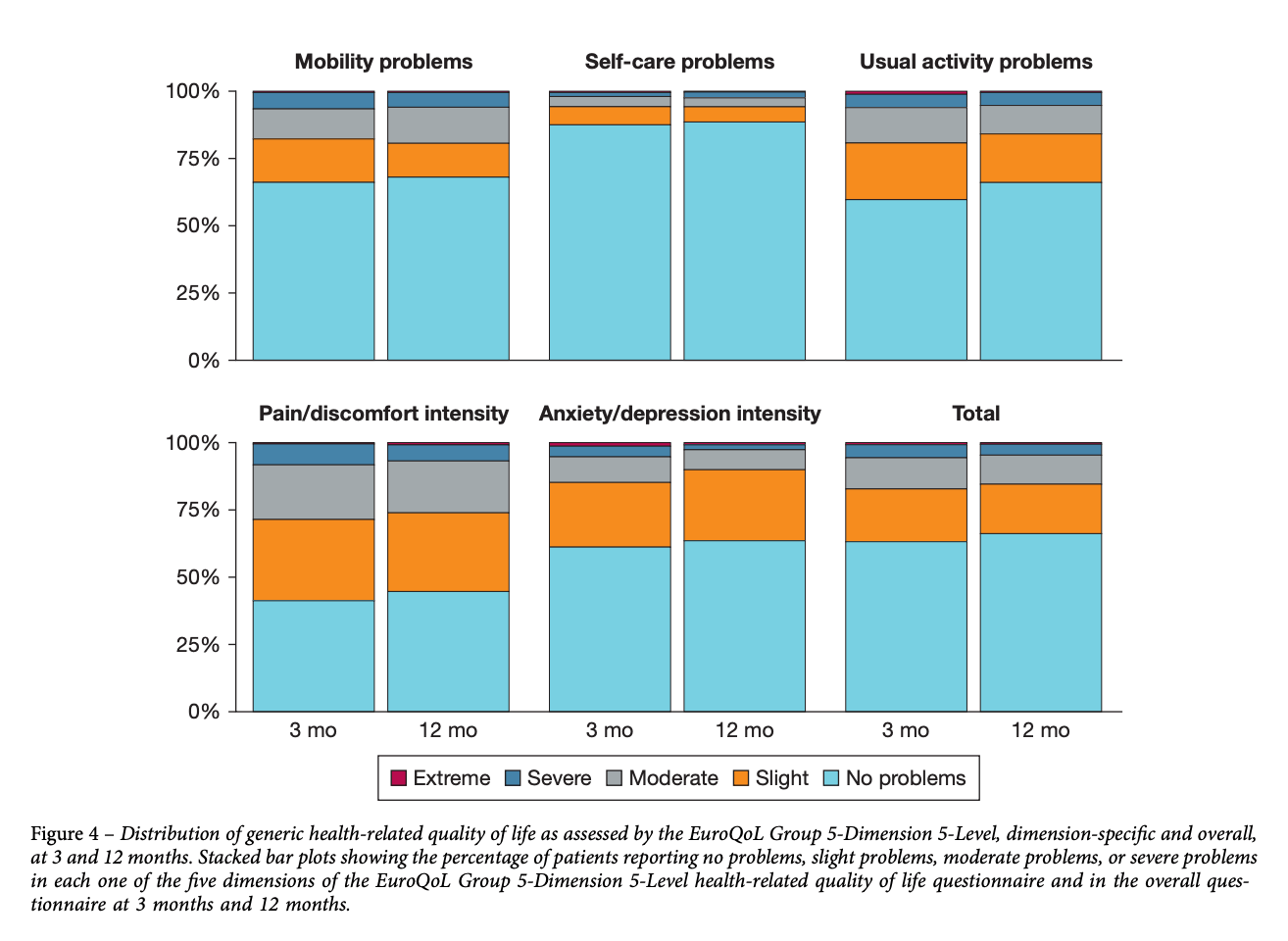
The annual incidence of acute pulmonary embolism (PE) has been increasing, along with progressively decreasing mortality. Many survivors have reported long-lasting and potentially severe symptoms or disability, affecting qualify of life (QoL). In a study in this month’s CHEST, Valerio and colleagues focused on finding the determinants of disease-specific and generic health-related QoL 3 and 12 months following an acute PE. They evaluated consecutive adult patients with objectively diagnosed PE, from the Follow-up after Acute Pulmonary Embolism study, who completed the Pulmonary Embolism Qualify of Life questionnaire at predefined visits 3 and 12 months following PE. The authors found that female sex, higher BMI, and preexisting chronic cardiopulmonary disease were associated with worse QoL at both 3 and 12 months. Over time, the association with BMI became weaker and QoL declined in older patients and those with a history of venous thromboembolism. Both disease-specific and generic health-related QoL improved between 3 and 12 months following an acute PE.