Hot in Journal CHEST: August 2020
By: Divya C. Patel (@divyacpateldo)
August 4, 2020
 Each month, we ask our Social Media Co-Editors of CHEST, to weigh in on the hot topics in CHEST. It's August, so let's hear from co-editor, Dr. Patel, as she outlines her highlights. After reviewing the issue, be sure to share your hot list on our Facebook, tweet with the hashtag #journalCHEST, or discuss in the CHEST LinkedIn group.
Each month, we ask our Social Media Co-Editors of CHEST, to weigh in on the hot topics in CHEST. It's August, so let's hear from co-editor, Dr. Patel, as she outlines her highlights. After reviewing the issue, be sure to share your hot list on our Facebook, tweet with the hashtag #journalCHEST, or discuss in the CHEST LinkedIn group.
This month, I am excited to highlight articles from outside my “comfort zones” to highlight great research being published in journal CHEST in the fields of asthma, point-of-care ultrasonography, and sleep medicine. Please also take a look at the General Interest Commentary and Announcements section in this month’s journal that highlight unique perspectives on the ongoing COVID-19 global pandemic. However, one of my favorite pieces to read this month was the medical history by Taghizadieh and others on asthma in which the authors trace the description of the disease 1,000 years ago to the work done by the physician Yaqub Kashkari. The article also includes some unique figures from a tenth century book on medicine describing asthma.
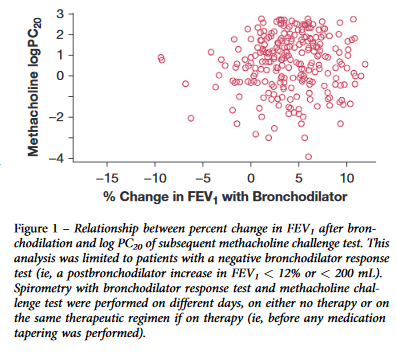
Asthma can be diagnosed either on spirometry with bronchodilator response (BDR) or methacholine challenge (MCT) testing. In this study, the Canadian Respiratory Research Network aimed to test the performance and reliability of these tests because the cutoff point for MCT can vary between guidelines. Data for this study were collected from a separate study of patients diagnosed by their physicians with asthma between 2012 and 2015. A total of 695 patients were enrolled and underwent spirometry with BDR testing and 500 patients underwent MCT. The study showed that 43% of patients with negative BDR findings had positive MCT findings, and those with prebronchodilator airflow obstruction were more likely to have a positive MCT. They also showed that bronchodilator tapering could impact MCT results, and the results could also spontaneously change. If the clinical suspicion of asthma is high, the authors recommended that MCT should be serially repeated.
Because pretest-probability of either exudative or transudative pleural effusion can affect the type of invasive procedure offered to a patient for management of pleural effusion, Shkolnik and colleagues tested whether thoracic ultrasonography (TUS) could be used to distinguish between the two types of effusion prior to the drainage procedure. In a single center, 285 consecutive patients with 300 pleural effusions were assessed using TUS prior to undergoing drainage. The researchers analyzed the sensitivity, specificity, positive predictive value, and negative predictive value of anechoic fluid for transudative effusion and complex fluid collection for exudative effusion. The study results showed that anechoic fluid is neither sensitive nor specific for transudative effusion. In addition, although complex effusions were highly likely to represent exudative effusion, 10% of patients with complex effusions without septations were transudative. However, they did show that the positive predictive value of septations for exudative effusion is 96%. They concluded that TUS does not reliably diagnose transudative or exudative effusion.
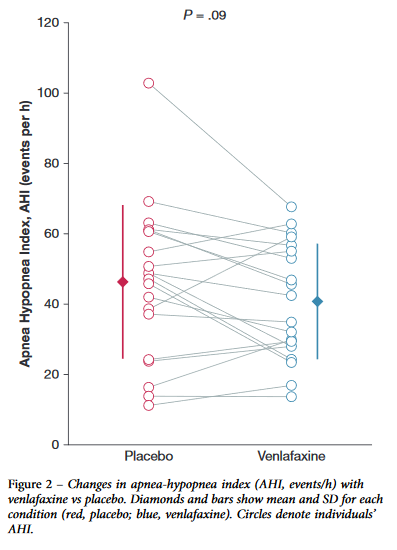
Because adherence to continuous positive airway pressure for treatment of obstructive sleep apnea (OSA) is poor, the authors of this study aimed to test venlafaxine as a pharmacologic treatment. This was because venlafaxine can increase noradrenaline levels, which may improve pharyngeal muscle tone and lead to decreased OSA severity. They performed a randomized, double-blind, placebo-controlled trial in which 20 patients with OSA underwent two polysomnograms at least four days apart and received either immediate-release venlafaxine 50 mg or placebo. The primary end point was changes in apnea-hypopnea index and oxygen saturation nadir. The study showed no improvement in the primary end points. The authors did show in a post hos analysis that, among patients with a high arousal threshold, the apnea-hypopnea index improved by 19%. They suggest additional clinical trials are needed with better patient selection or combination therapy.