Hot in Journal CHEST: August 2021
By: Viren Kaul, MD, FCCP
August 25, 2021
 Each month, we ask our Social Media Co-Editors of CHEST to weigh in on the hot topics in the journal CHEST®. It's August, so let's hear from Co-Editor Dr. Kaul as he outlines his highlights for this month. After reviewing the issue, be sure to share your hot list on our Facebook, tweet with the hashtag #journalCHEST, or discuss in the CHEST LinkedIn group.
Each month, we ask our Social Media Co-Editors of CHEST to weigh in on the hot topics in the journal CHEST®. It's August, so let's hear from Co-Editor Dr. Kaul as he outlines his highlights for this month. After reviewing the issue, be sure to share your hot list on our Facebook, tweet with the hashtag #journalCHEST, or discuss in the CHEST LinkedIn group.
I typically dive into the journal to learn more about an area I am comfortable with, a subspecialty of pulmonary, critical care, and sleep medicine that I feel a need to update myself in, and a topic that is outside my usual practice patterns. So, let's talk about the first article on my highlight list!
Methodologic Quality of Guidelines for Training or Competence Processes for Basic Point-of-Care Echocardiography in Critical Care: A Systematic Review of the Literature
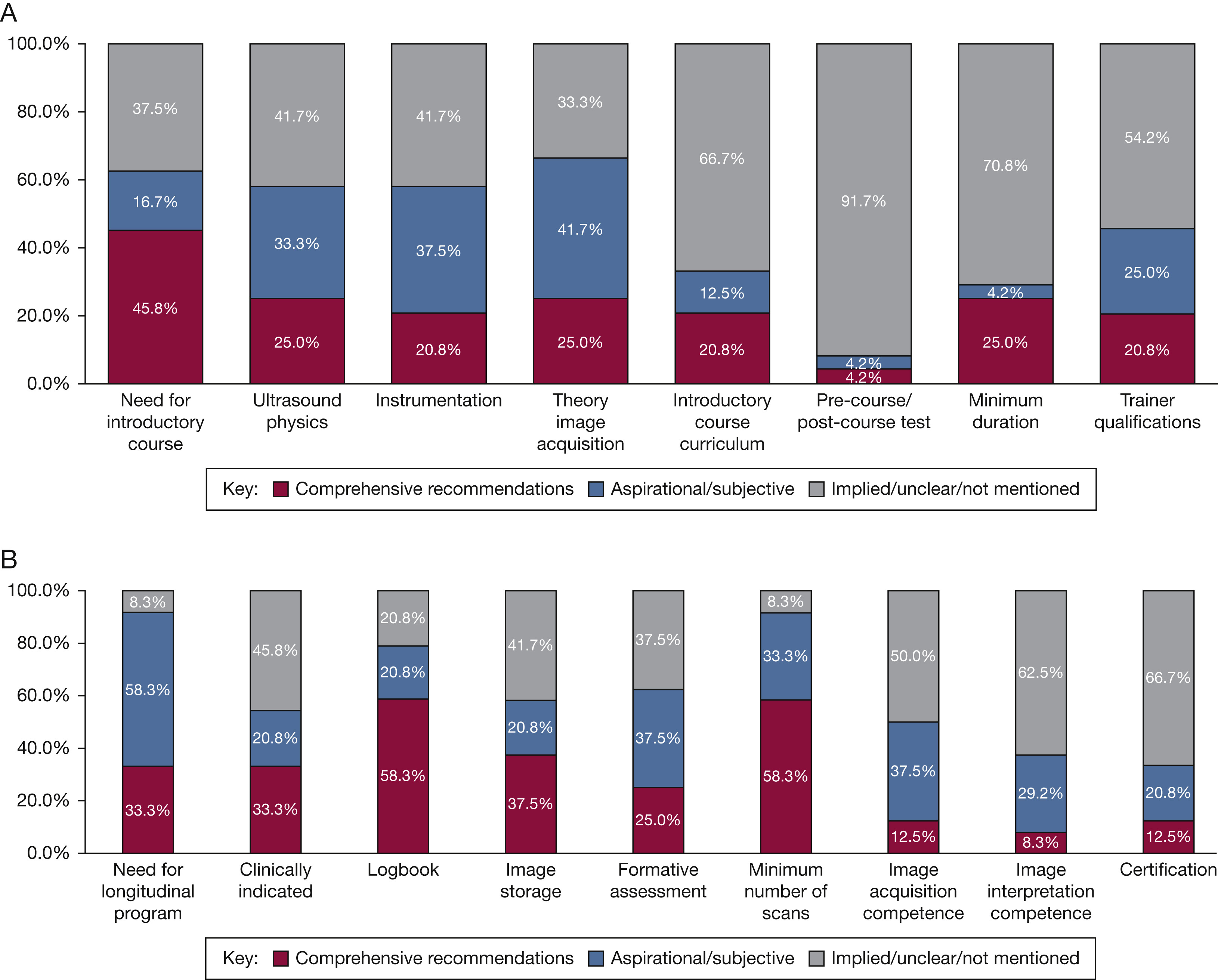
With the use of basic critical care echocardiography (BCCE) gaining acceptance and widespread use, it has become increasingly important to determine competence-based processes for training clinicians to use this modality. Rajamani and team evaluated 24 published guidelines or recommendations on training or competence processes for BCCE using the Appraisal of Guidelines for Research and Evaluation (AGREE-II) instrument.
They found that very few guidelines made clear recommendations regarding introductory courses, including the physics, instrumentation, course curriculum, testing, minimal course duration, or trainer qualifications, or for longitudinal competence programs, including aspects such as formative assessment, image acquisition, image interpretation, and credentialing or certification. Only one guideline attained greater than or equal to 75% in every domain of the AGREE-II score.
Their approach of using the AGREE-II score for grading these guidelines or recommendations based on "quality" is unique and applicable. This study highlights the gap in the training paradigm for point-of-care ultrasound and provides an opportunity for consideration of standardization of courses and training materials.
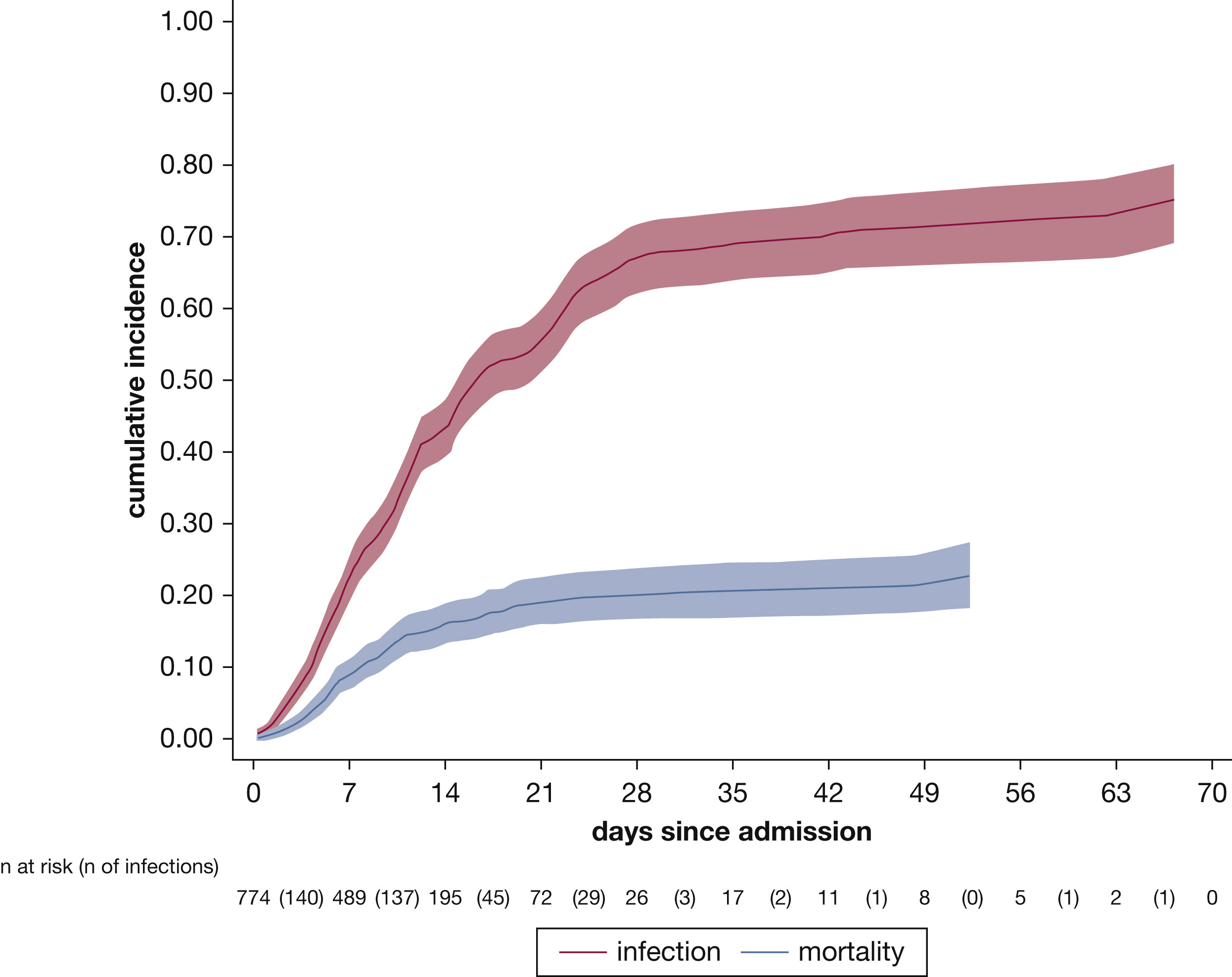
Hospital-Acquired Infections in Critically Ill Patients With COVID-19
In this study, the authors hammer down what clinicians have reported during the COVID-19 pandemic: That nearly 50% of patients critically ill with COVID-19 experience a secondary infection! Of these, a third of the infections are caused by multidrug-resistant organisms. This study starkly makes a point of careful consideration of antibiosis in patients with COVID-19 who have been described to get antibiotics often at the beginning of their course, followed by other regimens during their illness. The authors report that 68% of patients receive antibiotics at the time of ICU admission, while only 1% have a documented secondary infection.
This study highlights the importance of clinical discretion when prescribing antibiotics to patients critically ill with COVID-19, unless there is a clear indication of a secondary infection, since that is precisely how the spiral of antibiotic misuse, colonization, and selection of drug-resistant organisms and failure of antibiotics begins. Especially at the initial phase of ICU stay, the likelihood of a secondary infection/co-infection appears to be low. Thus, I will use this information to take a diagnostic time-out to deliberately consider the benefits of antibiotics, especially early in the course of critical illness with COVID-19.
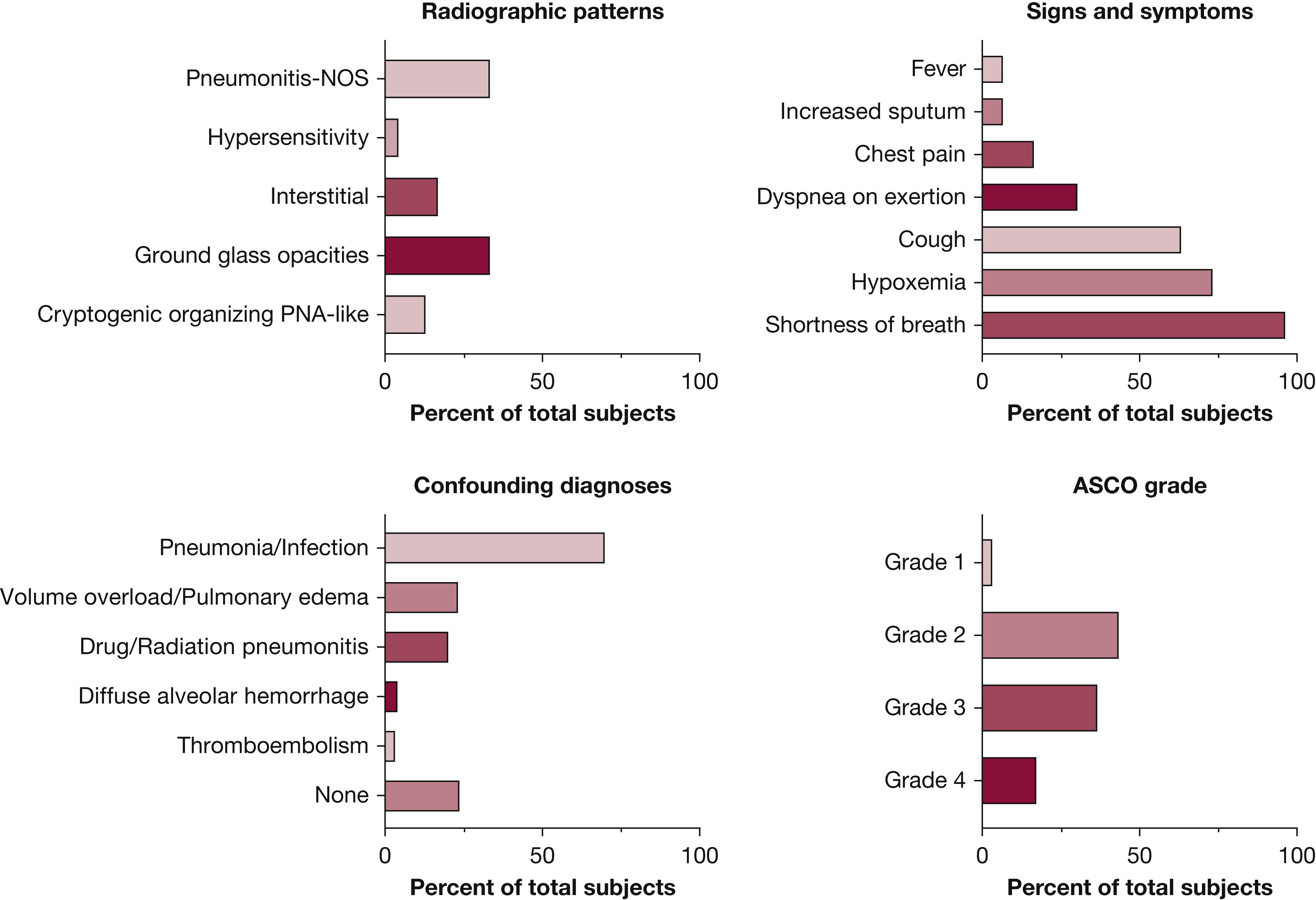
Immune Checkpoint Inhibitor-Related Pneumonitis in Lung Cancer: Real-World Incidence, Risk Factors, and Management Practices Across Six Health Care Centers in North Carolina
In this study, records of a real-world cohort of patients from six centers in North Carolina, United States, were reviewed to understand the risk factors, clinical presentations, radiological findings, and outcomes in patients who developed immune checkpoint inhibitor-related pneumonitis (ICI-P). The incidence of ICI-P was found to be 9.5%. Most patients had high severity of pneumonitis, and 27% of patients died while being treated for the ICI-P.
This study suggests that ICI-P is more common and more severe than previously reported. Chronic pulmonary diseases seem to confer an increased risk of ICI-P in this study. While I will be closely watching for a larger trial in this space, it does inform me to lower my threshold for diagnosis of ICI-P when evaluating patients on checkpoint inhibitors while on pulmonary service.
I hope you found these summaries helpful. Check out details on these studies in the August 2021 edition of the journal CHEST. I wish you, your families, and your colleagues the best of health over the coming months. On behalf of the journal's editorial board, please accept our gratitude for all your hard work on the front lines.