Hot in Journal CHEST: September 2021
By: Divya C. Patel, DO
September 2, 2021
 Each month, we ask our Social Media Co-Editors of CHEST to weigh in on the hot topics in CHEST. This month, Dr. Patel shares her highlights of the September 2021 issue. After reviewing the issue, be sure to share your hot list on Twitter with the hashtag #journalCHEST.
Each month, we ask our Social Media Co-Editors of CHEST to weigh in on the hot topics in CHEST. This month, Dr. Patel shares her highlights of the September 2021 issue. After reviewing the issue, be sure to share your hot list on Twitter with the hashtag #journalCHEST.
It has been some time since I last wrote this blog. I hope that you have enjoyed reading blog entries from my colleagues. The diversity of viewpoints and ideas is what makes our community and the journal CHEST® thrive.
Wherever you are practicing, I hope that you are not seeing the dramatic surge in COVID-19 cases that my institution has seen. It has been disappointing to see many young people ill. To combat burnout, I have been working hard to convince patients and their entire families to get vaccinated, including at point of care. Every time a patient agrees, I get a feeling of success and hope that I haven’t felt in some time. I feel like I am truly serving my community and country. Please continue to stay safe, and encourage patients to get vaccinated.
This month, I have purposefully chosen three articles that have nothing to do with COVID-19.
Clinical and Prognostic Impact of Low DLCO Values in Patients With GOLD I-Classified COPD
Several studies of moderate to severe COPD have shown that diffusing capacity for carbon monoxide (DLCO) values could help identify increased mortality in people with COPD. The Global Initiative for Obstructive Lung Disease (GOLD) recommendations also do not mention DLCO to determine severity or treatment strategies. Patients classified as GOLD stage I (mild airflow obstruction) have not been included in clinical trials given that people assume that since they have mild disease, prognosis is better. The authors of this study tested whether a DLCO measurement in patients within the GOLD I disease classification could help determine worse mortality.
Patients classified as GOLD I from three prospective COPD cohorts followed for an average of 9 years were evaluated. Multivariate analysis showed a DLCO cutoff of <60% predicted was associated with higher all-cause mortality. The patients also had lower BMI, worse dyspnea, and a higher BODE score.
This study shows that even patients with “mild” obstruction can have a poor prognosis. A DLCO value can help identify patients at risk.
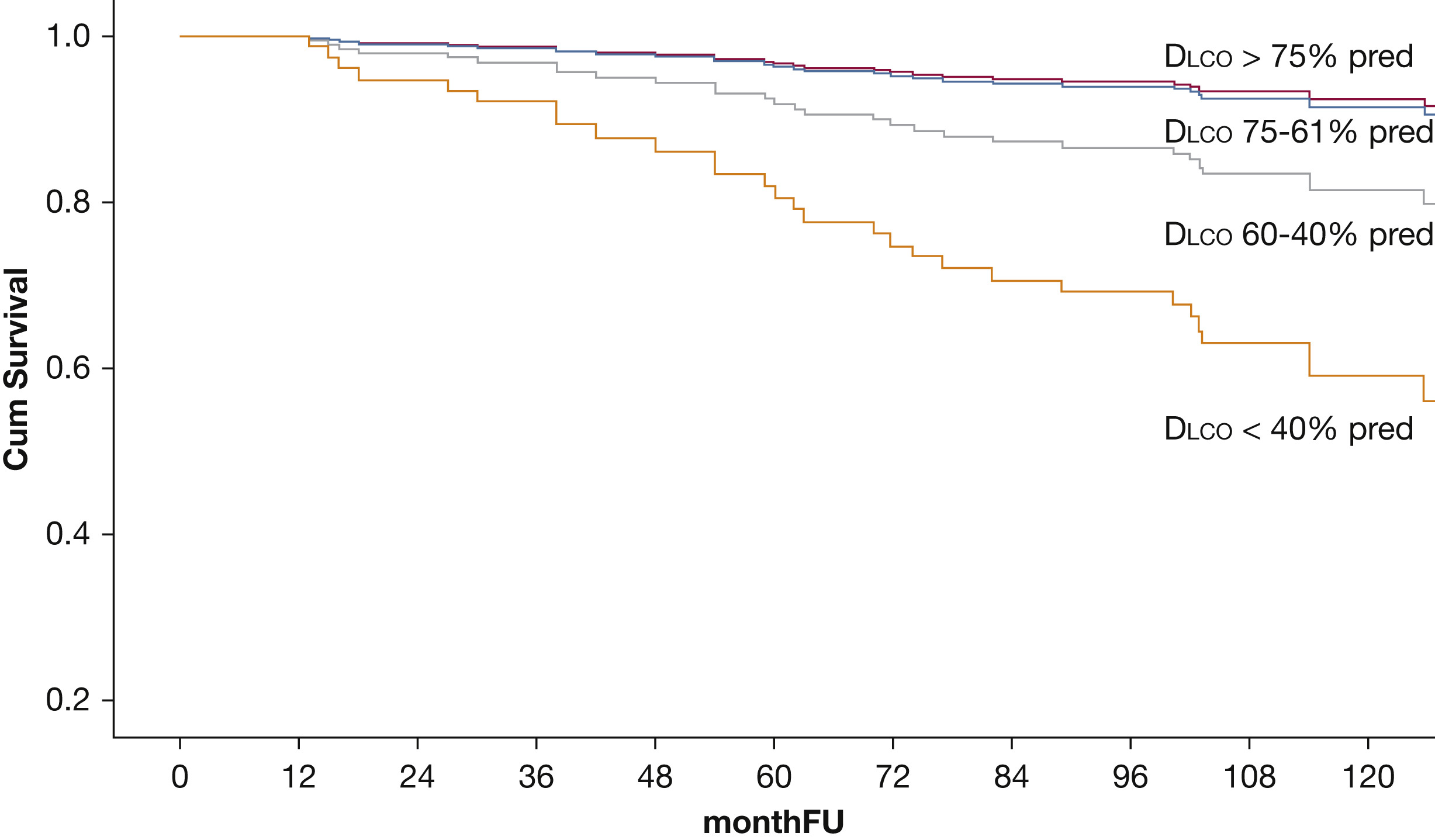 Figure 1. Survival curves of each of the ERS/ATS guidelines DLCO categories (>75%, 75-61%, 40-60% and <40% of predicted values) adjusted by age, sex, pack-years history, smoking status and BMI.
Figure 1. Survival curves of each of the ERS/ATS guidelines DLCO categories (>75%, 75-61%, 40-60% and <40% of predicted values) adjusted by age, sex, pack-years history, smoking status and BMI.
254x190mm (96 x 96 DPI)
A Mobile Health Intervention to Increase Physical Activity in Pulmonary Arterial Hypertension
In this study, the investigators wanted to determine if unsupervised physical activity intervention using a text-based strategy increases step counts in patients with pulmonary arterial hypertension (PAH).
It has been established that supervised exercise programs can help improve exercise capacity in patients with PH. However, supervised exercise programs, such as pulmonary rehabilitation programs, are not widely available or affordable for patients.
A randomized, single-blind trial was performed to determine mean step count at week 12. Patients in the intervention arm received three automated encouraging text messages per day with a real-time step count. Forty-two patients were randomized, and the results showed that an increase in step counts from baseline to week 12 was higher in the intervention arm. The intervention arm also took a higher number of steps on all days between day 9 to 84. However, no difference in 6-minute walk distance was detected between the two groups.
This study shows that an unsupervised exercise program that includes an activity tracker with daily encouragement leads to higher total step counts.
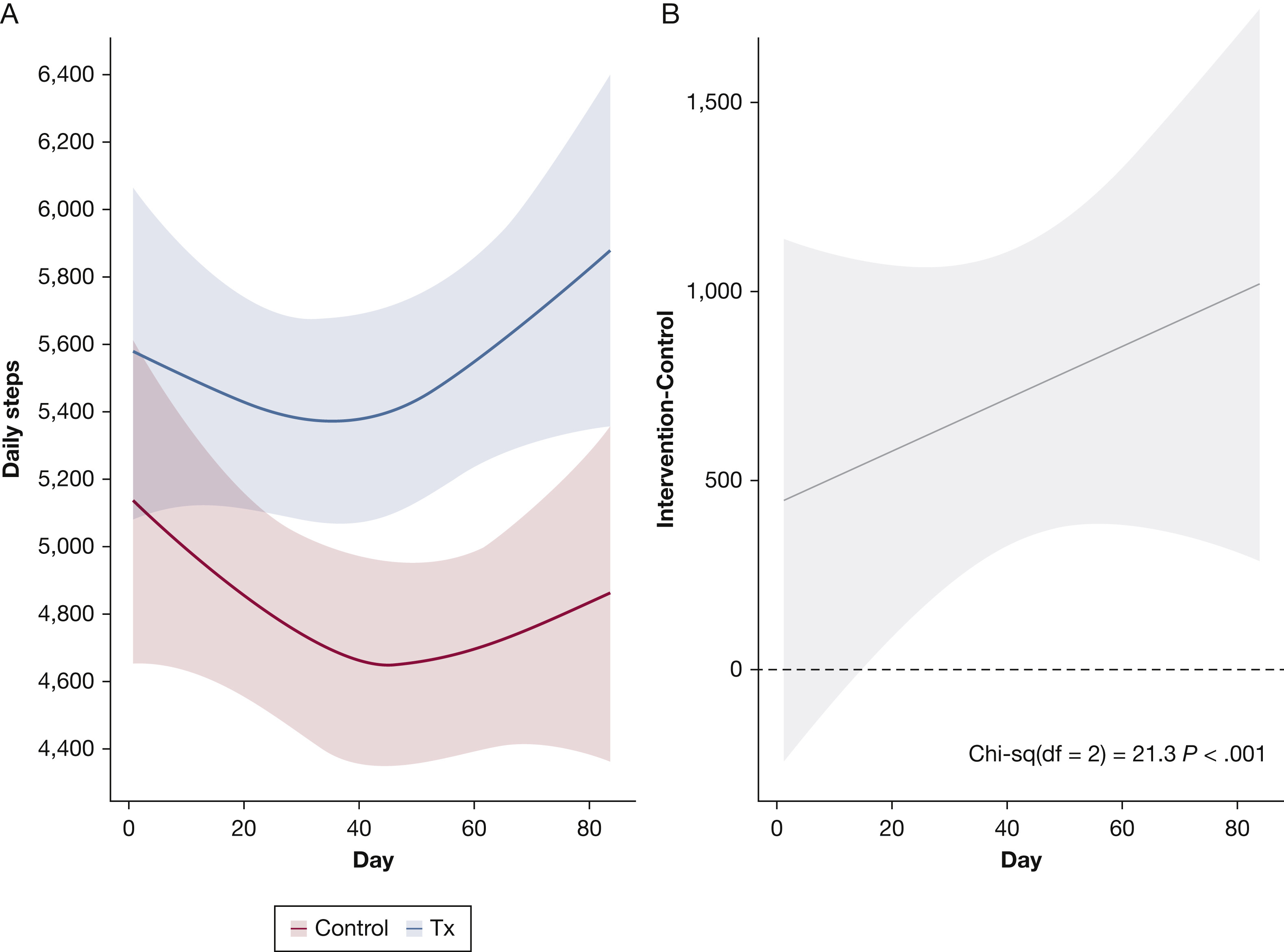 Figure 2. Effect of the Mobile Health Intervention on Daily Step Counts over 12 Weeks.
Figure 2. Effect of the Mobile Health Intervention on Daily Step Counts over 12 Weeks.
165x119mm (72 x 72 DPI)
Incidence and Prognostic Significance of Hypoxemia in Fibrotic Interstitial Lung Disease: An International Cohort Study
Hypoxemia is common in patients with fibrotic interstitial lung disease (ILD), and when present with exertion, is associated with higher mortality. However, the incidence, progression, and prognostic implications of hypoxemia in this cohort are unknown, so the investigators utilized registries from ILD centers in three countries to answer this question. Eight hundred forty-eight patients with baseline and serial 6-minute walk tests and arterial blood gases were included. Cumulative incidence of exertional hypoxemia at 5 years was reported as 40.1% and 16.5% for resting hypoxemia. Patients with idiopathic pulmonary fibrosis (IPF) had a higher incidence of hypoxemia than patients without IPF.
Interestingly, the authors added exertional or resting hypoxemia to the GAP score model for 1-year mortality, and it showed improved prediction.
This study provided incidences of exertional and resting hypoxemia in patients with and without IPF. It also demonstrated that adding information about hypoxemia to the GAP score improved its ability to predict mortality at 1 year.
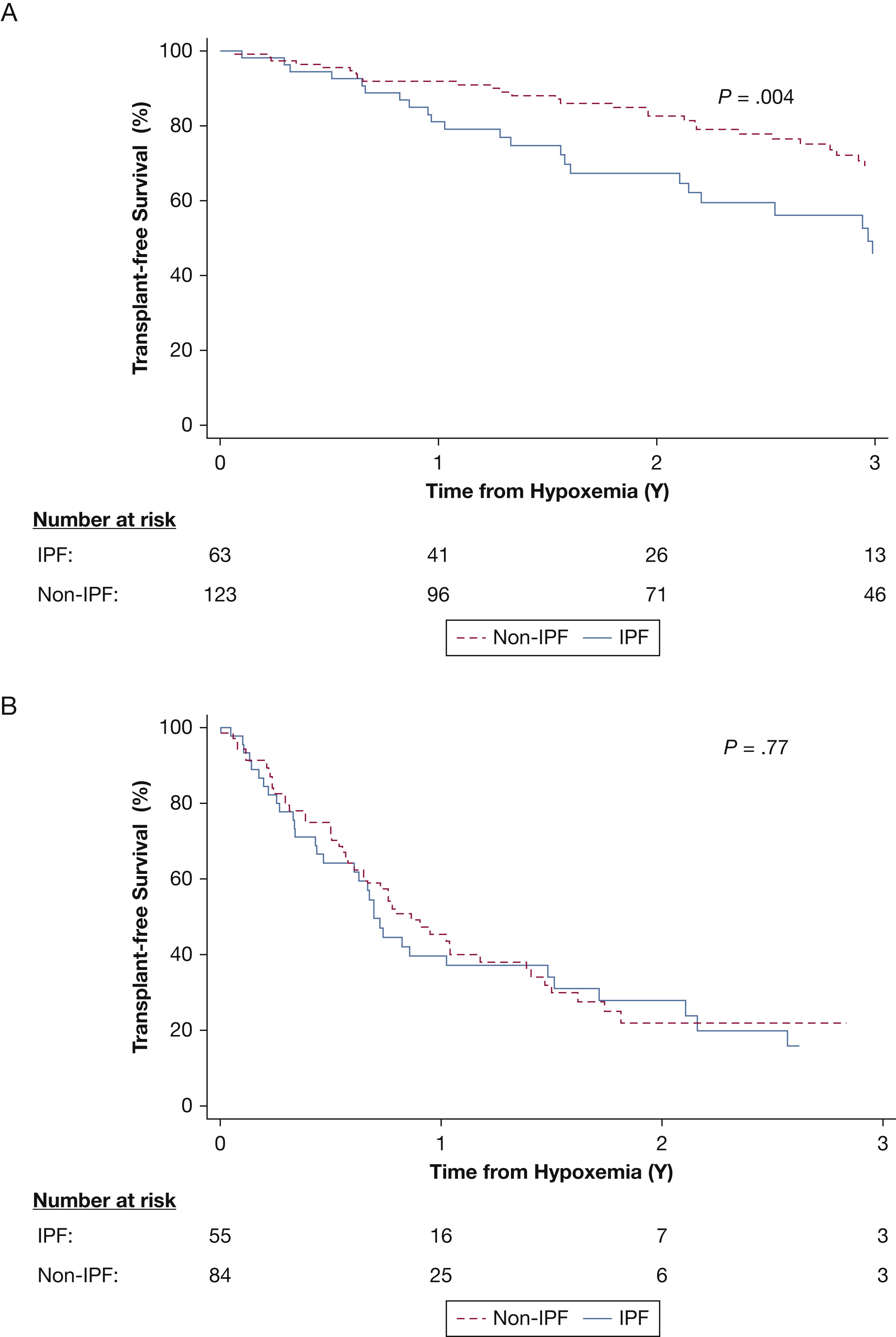 Figure 3a. Kaplan-Meier survival curve following new-onset exertional hypoxemia.
Figure 3a. Kaplan-Meier survival curve following new-onset exertional hypoxemia.
Abbreviation: IPF, idiopathic pulmonary fibrosis
95x71mm (300 x 300 DPI)