Hot in Journal CHEST October 2018
By: Viren Kaul, MD
October 2, 2018
 Each month, we ask our Social Media Co-Editors of CHEST to weigh in on the hot topics in CHEST. It's October, so let's hear from one of our new co-editors, Dr. Viren Kaul, as he outlines his highlights. After reviewing the issue, be sure to share your hot list on our Facebook wall, tweet with the hashtag #journalCHEST, or discuss in the CHEST LinkedIn group.
Each month, we ask our Social Media Co-Editors of CHEST to weigh in on the hot topics in CHEST. It's October, so let's hear from one of our new co-editors, Dr. Viren Kaul, as he outlines his highlights. After reviewing the issue, be sure to share your hot list on our Facebook wall, tweet with the hashtag #journalCHEST, or discuss in the CHEST LinkedIn group.
October is here! And that only means one thing: it’s time for #CHEST2018. Don’t forget to grab this month’s edition of CHEST® for your flight over to San Antonio. Of the many interesting studies and articles, here are the ones that caught my eye:
Efficacy of Dexamethasone in Preventing Acute Mountain Sickness in COPD Patients: Randomized Trial
Patients traveling to high altitudes (>3,000 meters) often seek prophylaxis for acute mountain sickness (AMS) and altitude-related adverse health effects (ARAHE) from their pulmonary and primary care physicians. No solid data exist regarding incidence or prevention of AMS/ARAHE in COPD. Dexamethasone has been shown to be effective in preventing AMS in healthy individuals and is used in treatment of exacerbations of COPD. If you ask me, it made complete sense to study this potential “double win” medication in patients with COPD looking forward to taking in those mountain vistas.
In this randomized, double-blind study conducted in Kyrgyzstan, Michael Furian and team report that while 4 mg twice a day of dexamethasone lessened altitude-induced hypoxemia, it was not superior to placebo for prevention of AMS/ARAHE in patients with mild to moderate COPD. Significantly higher number of patients developed hyperglycemia in the dexamethasone arm. Of note, lower levels of PaO2 at <760 meters did not appear to be protective against AMS/ARAHE in patients with COPD (as hypothesized in the past).
Despite proven efficacy in preventing AMS in healthy people, dexamethasone may not be the answer for patients with COPD! This study highlights the importance of continued research on prevention and treatment of AMS in patients with chronic lung diseases.
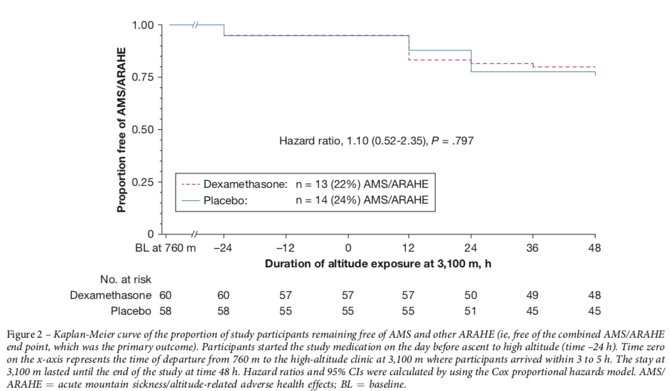
Furian M, Lichtblaum M, et al. Efficacy of dexamethasone in preventing acute mountain sickness in COPD patients: randomized trial. Chest. 2018;154(4):788-796.
Effect of Acute Exacerbation of Idiopathic Pulmonary Fibrosis on Lung Transplantation Outcome
Patients with idiopathic pulmonary fibrosis (IPF) who undergo acute exacerbations (AE-IPF) have high mortality, and lung transplantation can be life-saving. However, data are currently limited on long-term post-transplant survival and outcomes.
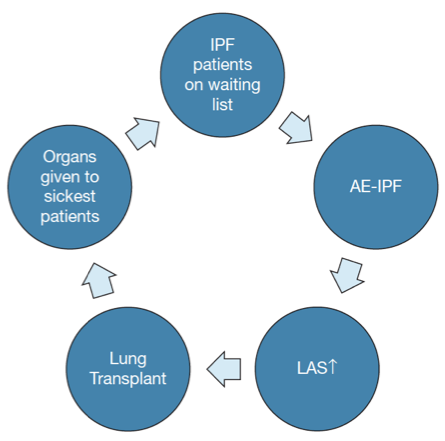
This single-center study by Dr. Yaniv Dotan’s group is the first to report significantly worse short (immediate) and long-term survival (1- to 3-year survival) in AE-IPF patients receiving lung transplant as compared with those IPF patients who were stable. It is notable that these patients do not die from pulmonary causes (eg, pneumonia) but from extrapulmonary chronic diseases and organ failure. Similar to other studies, the authors found that patients with lung allocation scores (LAS) more than 80 have lower survival both prior to and posttransplant.
These findings raise a serious ethical dilemma: Should the AE-ILD patients receive lung transplants? Transplanting the sickest patients (ie, patients currently with AE-ILD) causes patients with stable IPF (who have higher potential posttransplantation survival) to wait longer for organ allocation, thereby exposing them to the risk of developing AE-IPF over time and higher mortality before and after lung transplantation, creating a vicious cycle. Unfortunately, there is no clear answer here.
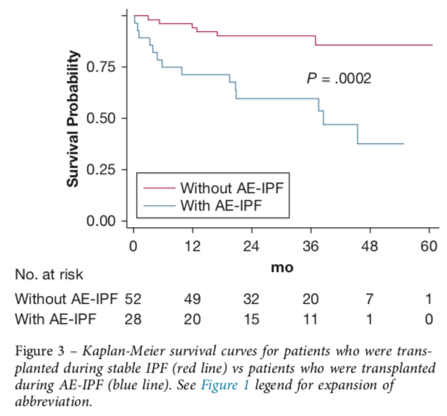
Dotan Y, Vaidy A, et al. Effect of acute exacerbation of idiopathic pulmonary fibrosis on lung transplantation outcome. Chest. 2018;154(4):818-826.
Left Atrial Volume as a Biomarker of Target Organ Damage in Cardionephrology: A Study in a Wide Range of Renal Function
The pathogenesis of cardiorenal syndrome (CRS) has been debated for a long time! In this innovative study, Dr. Zach Rozenbaum and his group describe the relationship of the four cardiac chambers’ volumes to the eGFR using a volumetric analysis of CT pulmonary angiograms.
Clinically decreased renal function has been described to be related to a dilated LA. The authors found that the LA volume index is associated with eGFR in an inverse manner, even with minimal renal dysfunction. Such a relationship has not been evaluated previously in patients with renal functions in ranges considered normal in clinical practice (eGFR, 60-89.9 mL/min/1.73 m2). Tripepi and colleagues previously demonstrated that LA volume adds an independent predictive value to mortality in renal dysfunction. Hence, the ability to assess this early onset cardiorenal dysfunction may allow screening and targeted treatment by using LA volume as a marker of target organ damage. Exciting stuff!
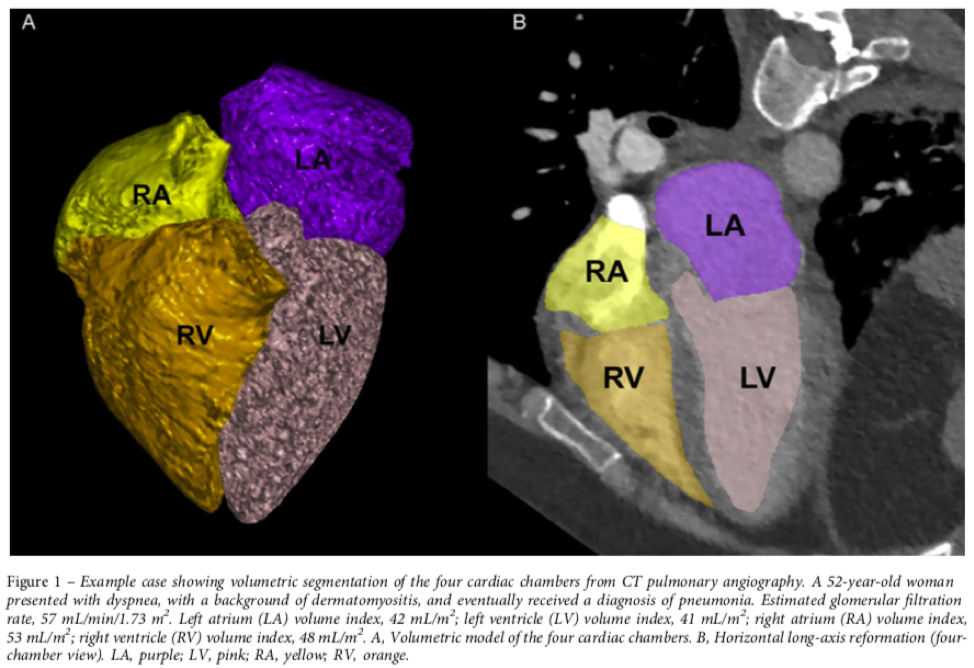
Rozenbaum Z, Ben-Bassat OK, et al. Left atrial volume as a biomarker of target organ damage in cardionephrology: a study in a wide range of renal function. Chest. 2018;154(4):893-903.