Hot Topics in CHEST January 2020
By: Viren Kaul, MD (@virenkaul)
January 15, 2020
 Each month, we ask our Social Media Co-Editors of CHEST to weigh in on the hot topics in CHEST. It's May, so let's hear from one of our co-editors, Dr. Kaul, as he outlines his highlights. After reviewing the issue, be sure to share your hot list on our Facebook wall, tweet with the hashtag #journalCHEST, or discuss in the CHEST LinkedIn group.
Each month, we ask our Social Media Co-Editors of CHEST to weigh in on the hot topics in CHEST. It's May, so let's hear from one of our co-editors, Dr. Kaul, as he outlines his highlights. After reviewing the issue, be sure to share your hot list on our Facebook wall, tweet with the hashtag #journalCHEST, or discuss in the CHEST LinkedIn group.
In the first 2020 issue of the journal CHEST®, I was impressed by the following three studies focused on ultrasonography and bronchoscopy. Before discussing what I learned from these articles, I would like to wish you a Happy New Year on behalf of the editorial board of the journal!
Let’s start with my top pick for this month:
A Randomized Trial of Nebulized Lidocaine, Lignocaine Spray, or Their Combination for Topical Anesthesia During Diagnostic Flexible Bronchoscopy
The authors ask a simple but elegant question: What’s the optimal strategy for topical anesthesia during bronchoscopy? The study subjects were divided into three groups: The first group received nebulized lignocaine, the second group received lignocaine oropharyngeal spray, and the third group received a combination of nebulized lignocaine as well as oropharyngeal lignocaine spray.
While the cumulative dose of lignocaine was least in the spray-only group, the patient and bronchoscopist-related cough severity scores were lower compared with the other groups. Even though the percentage of subjects undergoing endobronchial and transbronchial biopsies was relatively small, the spray-only group had better yield from the procedures.
What I found particularly useful is the fact that multiple bronchoscopists conducted the study procedures, and this makes the results generalizable. Personally, I do not use nebulized topical anesthesia for bronchoscopies and after reading this article, I plan on continuing my current practice of using topical spray as the preferred mode of topicalization. Let me know how this impacts your current practice in the comments below!
Accuracy of Several Lung Ultrasound Methods for the Diagnosis of Acute Heart Failure in the ED: A Multicenter Prospective Study
The use of lung ultrasound (LUS) has gained acceptance for evaluation of patients with dyspnea. However, there is uncertainty in terms of which protocol performs best for assessment of acute heart failure (AHF).
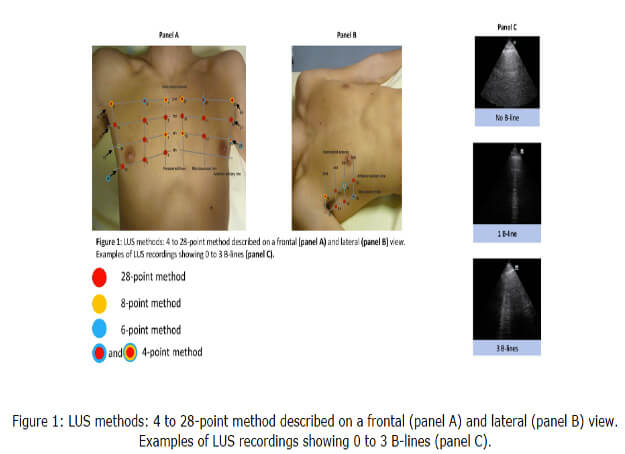
Overall, the 6- and 8-point exams used on top of the Brest score for AHF were the most discriminative, including in patients with intermediate Brest scores. The 4-point BLUE protocol, on the other hand, was found to have lesser diagnostic ability as compared with the other methods of LUS examination. The 28-point exam was found to have high sensitivity but low specificity.
This study informs the use of LUS when assessing for AHF by evaluating the various proposed LUS exams comparatively. I foresee further studies to validate these findings in other clinical settings from pre-hospital care to inpatient ICU and non-ICU settings. Is it time to move past the BLUE protocol when assessing for dyspnea and consider a 6- or 8-point exam as the standard?
Assessment of Diaphragm Function and Pleural Pressures During Thoracentesis
My final pick and certainly the one that had the physiology aficionado in me rejoicing! The authors of this study evaluate an innovative use for ultrasonography in pulmonary medicine: using M mode to measure the contraction velocity of the diaphragm as a method of assessing diaphragmatic function. They found increased diaphragm excursion and velocity of contraction during thoracentesis for pleural effusions with underlying expandable lung but not in cases where the lung was nonexpandable.
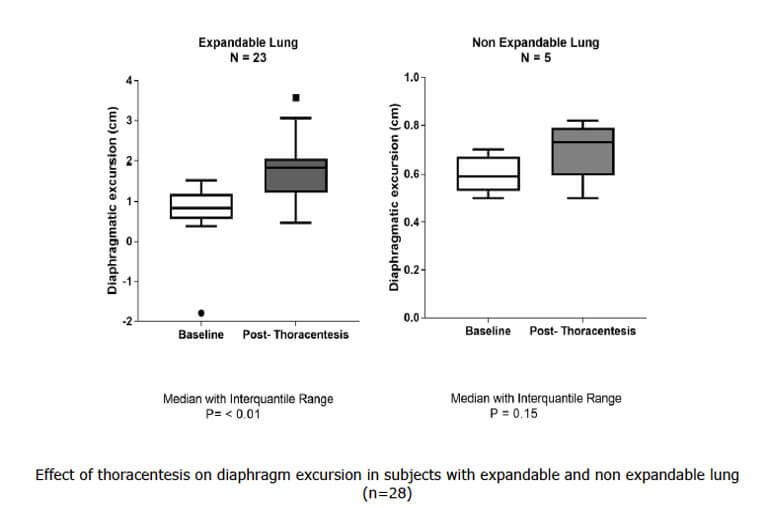
Even though this is a small study including only 28 patients, it does provide correlation to the physiology of relief of dyspnea after removal of pleural effusions by improving chest wall-lung dynamics as well as improved diaphragmatic configuration. The clinical use of assessing diaphragmatic function using ultrasound needs further elucidation, however, the potential to identify nonexpanding underlying lung in cases of pleural effusion could have real-world utility; for example, in making an early decision to use lytics intrapleurally. Time will tell, but, such a neat study!
It was a challenge to select my top picks this month, and I’m sure you will find the other articles in the January edition of CHEST highly informative as well! I look forward to bringing you highlights from the journal as the year goes on. Here’s to wishing you all a productive, satisfying, and joyful 2020!