Hot in Journal CHEST: April 2020
By: Viren Kaul, MD (@virenkaul)
April 3, 2020
 Each month, we ask our Social Media Co-Editors of CHEST to weigh in on the hot topics in CHEST. It's April, so let's hear from one of our co-editors, Dr. Kaul, as he outlines his highlights. After reviewing the issue, be sure to share your hot list on our Facebook, tweet with the hashtag #journalCHEST, or discuss in the CHEST LinkedIn group.
Each month, we ask our Social Media Co-Editors of CHEST to weigh in on the hot topics in CHEST. It's April, so let's hear from one of our co-editors, Dr. Kaul, as he outlines his highlights. After reviewing the issue, be sure to share your hot list on our Facebook, tweet with the hashtag #journalCHEST, or discuss in the CHEST LinkedIn group.
Now more than ever, medicine is at the forefront of defending humanity. I sincerely believe that all health-care professionals would go through the rigors this pandemic has placed on us all over again. It’s what our profession has trained us to do. The courage, constitution, and character each and every one of you has demonstrated in fighting COVID-19 will define medicine for generations to come. I am proud and humbled to be your colleague and know that, together, we will persevere. We will persevere and rebuild in time. Until then, my sincere gratitude to you all.
The April issue of the journal CHEST® provided a welcome relief, and I was reminded that life is still marching on. I’d like to summarize three studies that stood out because they address situations we have all faced in daily practice. The first study pertains to the hotly debated issue of contrast-associated acute kidney injury (AKI).
Association of Contrast and Acute Kidney Injury in the Critically Ill: A Propensity-Matched Study
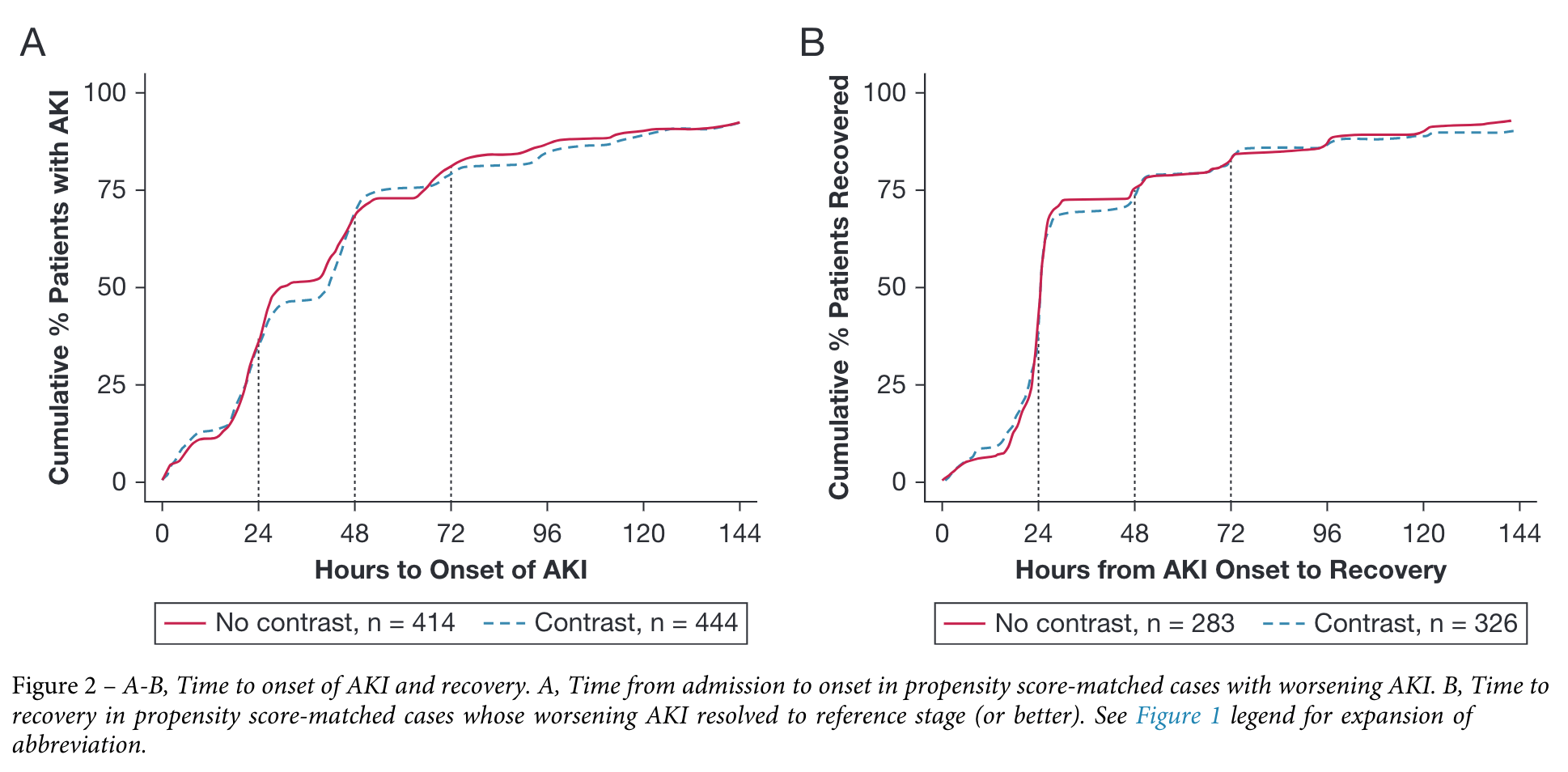
This publication by Williams and colleagues is a propensity score-matched study that compared 2,306 matched pairs of patients in the ICU who were exposed to IV iodinated contrast medium within 24 hours of admission with those who weren’t exposed. IV contrast was not found to contribute to onset or worsening of AKI. This study adds weight to the burgeoning body of evidence that contrast-associated AKI may be not be as clinically concerning as previously thought.
Sepsis, metabolic disorders, diabetes, history of renal disease, and severity of illness were noted as factors that were more strongly associated with development of AKI. Thus, efforts should be made to mitigate these conditions for prevention of AKI in general. As one of the largest trials to date in critically ill patients, results of this trial will be helpful when weighing the impact (or lack thereof) of venous contrast on the kidneys versus the need for a particular imaging study.
Effect of Different Probes and Expertise on Interpretation Reliability of Point-of-Care Lung Ultrasonography
This elegantly conducted study evaluated interrater agreement and reliability between residents, fellows, and senior physicians as well as three commonly used probe types for assessing basic lung ultrasonographic patterns in neonates. Overall basic lung ultrasonography parenchymal signs had good interrater agreement and interpretation reliability.
Agreement was lower in residents and fellows compared with senior physicians, especially when using the nonlinear probes. Reliability was lower in residents compared with fellows and senior physicians. This is the first study that evaluated use of various probes, especially in relationship to operator experience level. Accordingly, I would encourage novice users to employ the linear probe for evaluation of lung parenchyma using ultrasonography. This study is unable to tease out what constitutes “adequate” experience or training. This particular aspect of ultrasonography science and education remains to be better understood to provide direction to training programs.
Extremes of Age Decrease Survival in Adults After Lung Transplant
Lehr and coauthors present the largest analysis of risk factors for posttransplant mortality in the era of the Lung Allocation Score. Age was the most significant risk factor for death after lung transplant. Risk factors for death included both extremes of age, increased creatinine levels, single lung transplant, hospitalization before transplant, and increased bilirubin levels. The effect of age on survival became more prominent as the time from transplant increased. The observed lowered survival in younger patients existed across all diagnosis groups, although, expectedly, a majority of younger patients had the diagnosis of cystic fibrosis. Risk factors were also different according to age, with social determinants of health affecting survival conspicuously in patients aged younger than 30 years.

However, the cause of reduced survival in the two age extremes is driven by different mechanisms, presenting opportunities for intervention by the transplant community. As we all are involved in transplant consideration for patients with advanced lung disease, understanding the factors contributing to the mortality of transplant recipients will help in counseling and referring these patients in our clinical practice.
Hope you find this issue of CHEST as applicable to your scientific endeavors and clinical work as I did. I leave you, your families, and loved ones with best wishes for health, safety, and fortitude in these difficult times. Godspeed!