Hot in Journal CHEST: May 2020
By: Divya C. Patel (@divyacpateldo)
May 8, 2020
 Each month, we ask our Social Media Co-Editors of CHEST, to weigh in on the hot topics in CHEST. It's May, so let's hear from our newest co-editor, Dr. Patel, as she outlines her highlights. After reviewing the issue, be sure to share your hot list on our Facebook, tweet with the hashtag #journalCHEST, or discuss in the CHEST LinkedIn group.
Each month, we ask our Social Media Co-Editors of CHEST, to weigh in on the hot topics in CHEST. It's May, so let's hear from our newest co-editor, Dr. Patel, as she outlines her highlights. After reviewing the issue, be sure to share your hot list on our Facebook, tweet with the hashtag #journalCHEST, or discuss in the CHEST LinkedIn group.
I am excited to start my journey as Social Media Section Editor with this blog post. I hope to use my posts to feature articles from the monthly journal CHEST® issues that are exciting, practice changing, thought provoking or that highlight disparities. I believe that the role of the journal is to create conversations around ideas presented in publications, so I hope to hear from you.
I picked three patient-centered articles to highlight from this issue of the journal.
Geographic Analysis of Racial Disparities in Use of Pulmonary Rehabilitation After Hospitalization for COPD Exacerbation
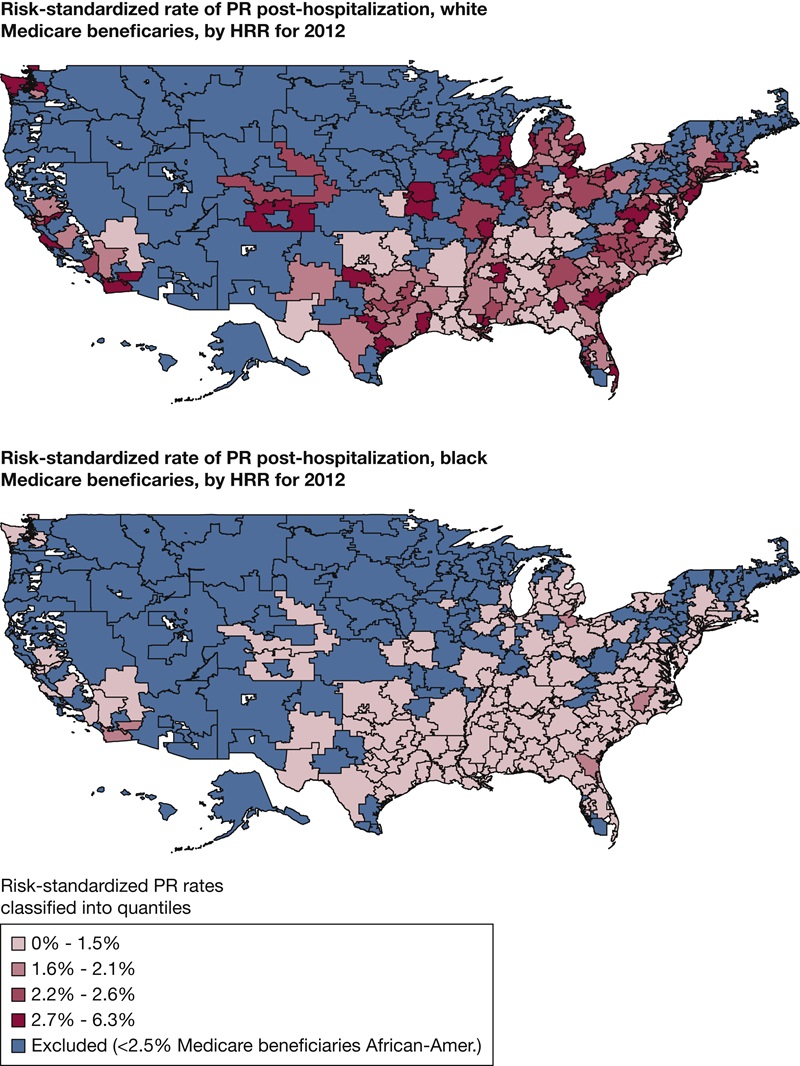
One of the most cost-effective ways to improve patient outcomes in those with COPD is to refer them to pulmonary rehabilitation (PR), and guidelines recommend PR 3 to 4 weeks after hospital discharge. Race and location have been shown to be associated with PR participation. Blacks and those residing in rural counties are less likely to participate in PR. This study aimed to determine if differences in access to PR contributed to racial differences in PR use.
The authors used US Centers for Medicare & Medicaid Services beneficiary files of those hospitalized for COPD in an acute care hospital in 2012 and who qualified for PR within 6 months of discharge. They used hospital-referral regions as the unit of analysis and determined the density of PR programs and estimated rates of PR. The authors showed that the median number of PR programs per 100,000 was 0.06. With regard to race, for non-Hispanic white beneficiaries, the density of PR programs was indeed linearly associated with PR rates but not for blacks. The authors stated that the disparity in rate of PR participation was not explained by location and PR program density. Black beneficiaries consistently had lower PR use than the national average, regardless of where they lived.
I was very surprised by these findings. However, disparities in care and access are seen across the spectrum in various disease states, and this paper helps us understand that disparity is not related to location and that we need more work in this area to close the gap.
Disease Severity and Quality of Life in Patients With Idiopathic Pulmonary Fibrosis: Cross-Sectional Analysis of the Idiopathic Pulmonary Fibrosis Prospective Outcomes Registry
This study utilized data collected in the US-based, multicenter Idiopathic Pulmonary Fibrosis (IPF) Prospective Outcomes registry, which includes patient data and quality of life (QOL) measured at 6-month intervals. The authors used data from 859 enrollees with IPF and aimed to determine whether there are associations between measures of IPF severity (Gender-Age-Lung Physiology [GAP] index and Composite Physiologic Index [CPI]) and QOL data (St. George’s Respiratory Questionnaire [SGRQ], Cough and Sputum Assessment Questionnaire, European Quality of Life-5 Dimensions, 12-Item Short Form [SF-12]).
The authors showed that, overall, patients with IPF have poor QOL scores, the correlation between the QOL scoring systems was modest at best (best for SGRQ and SF-12 physical component score), and that those with the highest GAP and CPI scores had worse QOL.
Interestingly, the authors also showed that within-patient GAP and CPI score correlation was modest at best, so the two scoring systems may be providing different information about the severity of IPF.
Thirty-Day Spending and Outcomes for an Episode of Pneumonia Care Among Medicare Beneficiaries
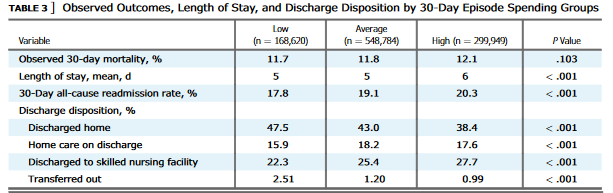
The authors of this study aimed to determine whether higher spending is associated with better outcomes for patients admitted to the hospital for pneumonia. In order to study the relationship, they looked at differences between spending on a 30-day episode of pneumonia care (including in-hospital and postdischarge care) and outcomes for Medicare beneficiaries. The 30-day episode of care metrics are important because they are part of the Hospital Value-Based Purchasing Program, a pay-for-performance initiative that rewards or penalizes acute care hospitals for outcomes for conditions like pneumonia.
After accounting for differences in patient and hospital characteristics, the authors found that there is no difference in mortality based on how much a hospital spends in a 30-day episode of pneumonia care in Medicare beneficiaries. They noted that this has not been the case for other conditions, such as acute myocardial infarction and heart failure, where higher spending has been associated with better outcomes. The authors also rightly pointed out that severity of illness was not taken into account in this study as a limitation. They also were not able to address how some hospitals were able to spend less and achieve the same results.
These are challenging and stressful times for our profession. I want to highlight the CHEST COVID-19: Updates and Resources webpage. One of my favorite features on this page is the CHEST Voices From the Community, where you can watch first-hand experiences of other health-care professionals throughout the country. Be well, colleagues.