Hot in Journal CHEST: December 2020
By: Divya C. Patel (@divyacpateldo)
December 29, 2020
 Each month, we ask our Social Media Co-Editors of CHEST, to weigh in on the hot topics in CHEST. It's December, so let's hear from co-editor, Dr. Patel, as she outlines her highlights. After reviewing the issue, be sure to share your hot list on our Facebook, tweet with the hashtag #journalCHEST, or discuss in the CHEST LinkedIn group.
Each month, we ask our Social Media Co-Editors of CHEST, to weigh in on the hot topics in CHEST. It's December, so let's hear from co-editor, Dr. Patel, as she outlines her highlights. After reviewing the issue, be sure to share your hot list on our Facebook, tweet with the hashtag #journalCHEST, or discuss in the CHEST LinkedIn group.
It is hard to believe that 2020 is coming to an end. It has been a challenging year for the world. Our personal lives and work lives have changed dramatically in a short amount of time. Many have lost loved ones to the COVID-19 pandemic, and many health-care workers are feeling the strain of overextended hospitals. Trust in science, medical care, and government institutions has been challenged by politics. Racial and socioeconomic disparities have become clearly evident to many in the US and around the world. However, we have also witnessed how science can bring hope, with the first vaccine for the SARS-CoV-2 virus developed, tested, and approved within the span of year. What an incredible achievement!
This month I want to highlight the great contribution of our international colleagues to the journal CHEST®. I’ve selected three articles that highlight the work of these colleagues in this month’s issue.
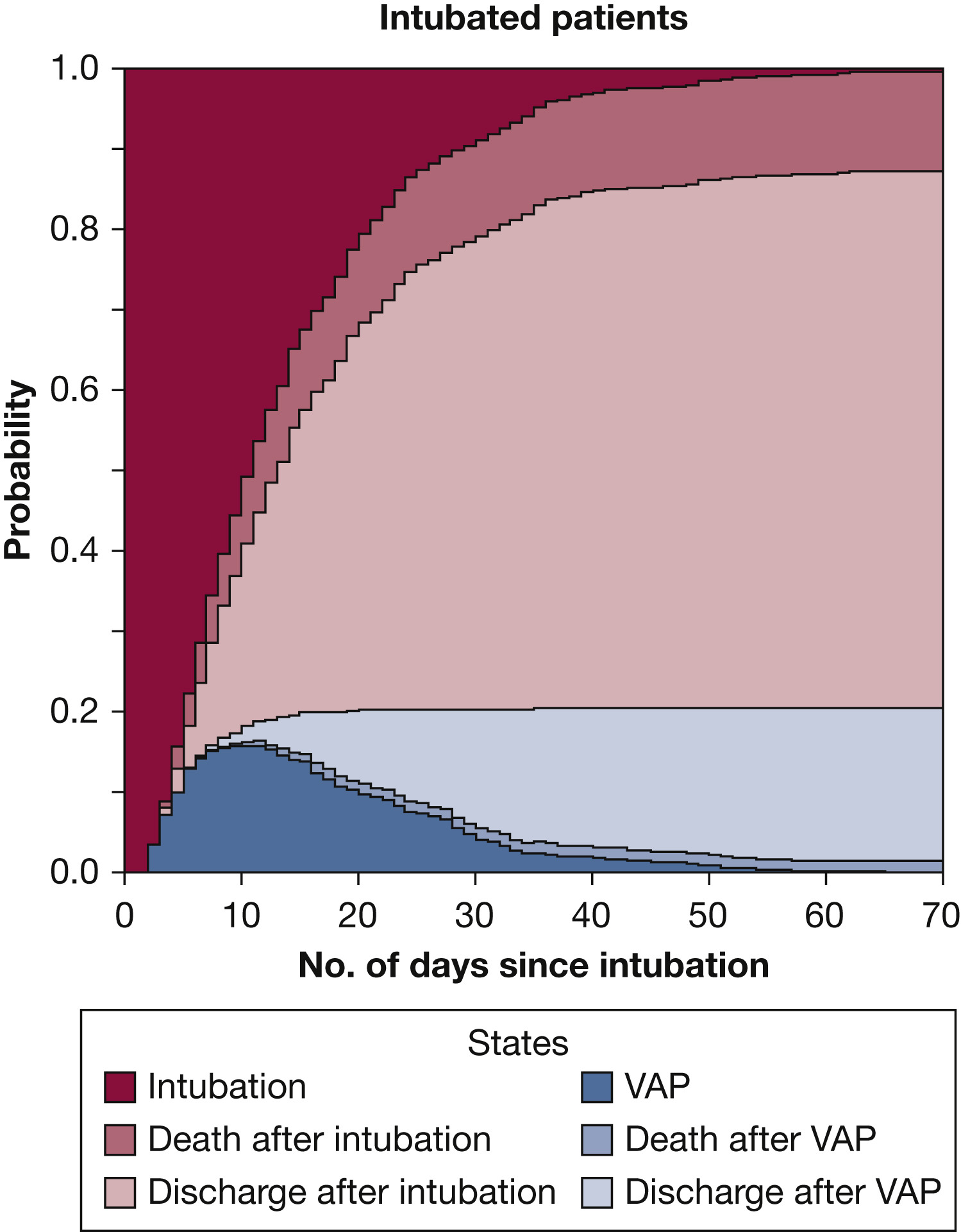
Ventilator-associated pneumonia (VAP) is common in critically ill patients on the mechanical ventilator, and patients with traumatic brain injury (TBI) who oftentimes require prolonged mechanical ventilation may particularly be at higher risk. The incidence, risk factors, and outcomes of patients with TBI were studied using the Collaborative European NeuroTrauma Effectiveness Research in Traumatic Brain Injury (CENTER-TBI). This analysis of the multicenter, longitudinal, prospective data set from 63 centers in Europe was preplanned. Patients admitted to the ICU within 24 hours of TBI and mechanically ventilated for at least 48 hours were included. Twenty percent of the 962 patients developed VAP. These patients were younger and had a higher incidence of alcohol/drug abuse, more frequent chest trauma, and more frequent respiratory failure. Risk factors for VAP include age, thoracic trauma, histamine-receptor antagonist intake, and antibiotic prophylaxis. Although the patients with VAP had a longer duration on the ventilator, it was not associated with increased mortality. The authors concluded that VAP occurred less often than previously described in patients after TBI.
Home mechanical ventilation (MV) is frequently required in patients with progressive neuromuscular disorders (NM) and is universally initiated in the hospital setting. However, this can be costly and use up limited bed space in hospitals. Previous studies have shown that MV initiated at home is feasible and less expensive than in the hospital. A national multicenter study in the Netherlands tested whether initiation of home MV with telemonitoring is noninferior to hospital initiation of MV in patients with NM and thoracic cage disorders. The primary outcome was a change in arterial PaCO2 over 6 months compared to baseline. A majority of the 96 randomized patients had NM disorders, and the study showed a significant improvement in PaCO2 in both groups and no significant differences between the groups. A secondary outcome analysis showed a significant cost reduction in the home MV group but no difference in quality of life measures. The authors concluded that from a patient perspective, initiation of MV at home might be an even more attractive approach.

Reduced exercise capacity is common in pulmonary Langerhans cell histiocytosis (PLCH), but the exact mechanism of this is unclear. Some have theorized that it is related to ventilatory limitations, such as dynamic hyperinflation (DH), and circulatory limitations, such as pulmonary hypertension (PH) and impaired gas exchange, as seen on cardiopulmonary exercise testing (CPET). The authors studied these mechanisms of exercise limitation in patients with PLCH by utilizing a CPET, 6-minute walk test, and right heart catherization (RHC). A total of 35 patients were enrolled in the study. Ventilatory and impaired gas exchange were the most common causes of limitations, but 71% had multiple reasons for impairment. Reduced DLCO was most frequently seen on pulmonary function testing. Prevalence of PH was 41% with a precapillary pattern.
