How APPs Helped Bridge the Staffing Gap During the COVID-19 Crisis
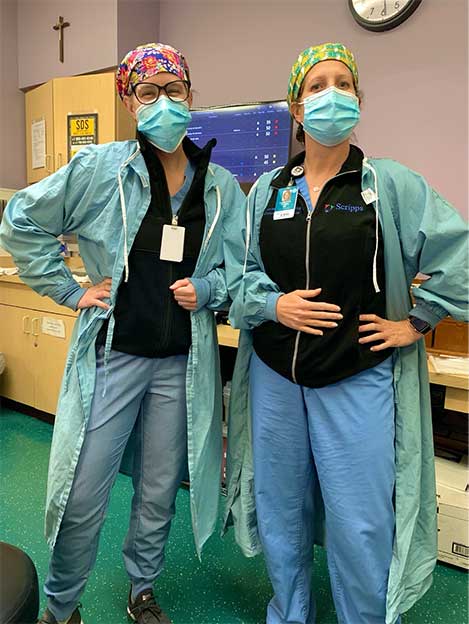
By: Charlotte Thomas, DNP-DNES, RN, AGACNP-BC, CCRN, and Sarah Norton, MSN, RN, AGACNP-BC, CCRN
February 5, 2021
Charlotte couldn’t figure out how this last-minute assignment offer for San Diego came about for her husband, an active-duty Naval Officer. His prior assignments had been in less “desirable” locations, compared to this place with amazing weather.
But arriving in Southern California from the Washington, DC area to be the first full-time nurse practitioner (NP) in the ICU at a Catholic charity hospital near the US-Mexico border almost 2 years ago was its own challenge, with its own growing pains. When the COVID-19 pandemic began, it became clear why she was needed: Augmentation was so desperately needed for these physicians on the front lines of one of the hardest-hit areas in the United States.
Our hospital is not a “glamorous” one full of technology and devices like ECMO, VADs, or transplant—it is a bread-and-butter, mostly medical, sometimes surgical ICU for an underserved and under-resourced community whose members have tremendous difficulties accessing health care. It is usually soul-revitalizing work, as the patients and families are grateful and appreciative every single day.
However, recruiting for our ICU is challenging despite the very close-knit and supportive staff and the true sense of camaraderie. Throughout the COVID-19 pandemic, we have struggled with physicians becoming ill themselves, with resignations, and with trying to hire outside of the timing for fellowship graduation. With a paucity of full-time intensivists, we were not staffed for the sudden influx of critically ill COVID-19 patients despite a quick expansion of the ICU bed count. The establishment of the NP program in our ICU the year before proved to be one of the key factors in maintaining our unit and providing care during this expansion in demand.
As the sole full-time NP who was working up to 25 shifts a month, however, Charlotte was emotionally and physically spent. By June 2020, it became clear there was a need for additional advanced practice providers (APPs). Sarah applied, and it was immediately evident she was the perfect fit; however, Sarah was also coming into the position tired, burnt out, and rundown after years of night shift work as a neurocritical care NP.
Entering into this ICU under these circumstances brought a new challenge she hadn’t realized she was ready to face. She was looking for the ability to grow her skills as an APP in a broader sense, and she was immediately brought fully into a whole new, multiorgan failure world head-on.
Working together, we developed firm guidelines and protocols as we managed half of the expanded ICU’s patients, alternating handoffs every few days to prevent further burnout as much as possible. At times, working in the COVID-19 ICU feels as if we have the same devastating conversations over and over again; therefore, preventing compassion fatigue has become paramount.
We have now added another two full-time NPs 10 months into the pandemic. This gives us two full NP shifts every day and greater depth in both our coverage and our experience level. We have worked to try to prevent burnout in these new expanded roles by limiting stretches of workdays to no more than five, having frequent check-ins, and maintaining an exceptionally cheeky group chat via text message. We have turned our shared ICU office into a Zen cave (complete with low lighting and aromatherapy for grounding, rebalancing, and renewal), which is helpful after daily phone calls to our patients’ families. What we have found the most helpful throughout this experience is the support we provide to each other as we work around a shared vision of patient-centered, evidence-based, quality care delivery.
 Charlotte Thomas, DNP-DNES, RN, AGACNP-BC, CCRN, is the Director, Advance Practice, at Scripps Health Inpatient Provider Medical Group and Chief, Advance Practice, Critical Care Medicine, at Scripps Mercy Hospital Chula Vista in Chula Vista, California.
Charlotte Thomas, DNP-DNES, RN, AGACNP-BC, CCRN, is the Director, Advance Practice, at Scripps Health Inpatient Provider Medical Group and Chief, Advance Practice, Critical Care Medicine, at Scripps Mercy Hospital Chula Vista in Chula Vista, California.
 Sarah Norton, MSN, RN, AGACNP-BC, CCRN, is an ICU nurse practitioner at Scripps Mercy Hospital Chula Vista in Chula Vista, California.
Sarah Norton, MSN, RN, AGACNP-BC, CCRN, is an ICU nurse practitioner at Scripps Mercy Hospital Chula Vista in Chula Vista, California.