How COVID-19 Turned Our Hospital—and Patients—Upside Down
By: Tyler Weiss, MSc, RRT, RRT-ACCS, AE-C
April 8, 2021
As COVID-19 started spreading throughout the United States, my colleagues and I didn’t know what to expect. Our hospital, Rush University Medical Center, is in the large metropolitan city of Chicago, so we assumed we would be hit hard. And as a respiratory therapist (RT) preparing for a respiratory pandemic, I knew my staff and I would be put to the test. We are used to caring for patients who require a high level of ventilator support: It’s not uncommon to have 25 to 35 patients requiring mechanical ventilation at a time at my institution, so the RTs stay fairly busy. If there was a team of RTs built to take down COVID-19, it was my team at Rush.
 The author and his nursing colleague (and fiancée) created a new manual prone positioning process.
The author and his nursing colleague (and fiancée) created a new manual prone positioning process.
As we prepared, we realized we needed a new process to prone patients, since this was one therapy that was being reported to help patients with COVID-19 who develoed ARDS. Prone positioning was not unfamiliar to my institution, as we would prone a handful of patients a year utilizing an automated bed. However, the automated process was not going to be feasible with the expected volume of patients.
My most trusted nursing colleague (who also happens to be my fiancée), Flor, and I created a new manual prone positioning process to be implemented immediately. Over the next couple of days, we created a YouTube video, order set, protocol, and checklists to support the new process while also training every RT and all ICU registered nurses throughout the hospital. We were ready!
The First Patient Arrives
As soon as we finished creating this new proning process, we were faced with our first critically ill patient with COVID-19 who required intubation and proning. It was March 18, 2020, and it marked the beginning of a time I will never forget. Flor and I, along with a couple other clinicians, did the honors and proned the patient. Our new process was put to the test, and it worked. Little did we know that the maneuver we just performed would be repeated throughout the year on more than 300 patients.
Over the next 2 weeks, we proned 42 patients. Soon, whole ICUs were filled with intubated patients requiring prone positioning, and we realized we weren’t as ready as we thought. The RTs were spread razor thin, as were the nurses, and we saw a whole new level of acuity and patient volume that was unfamiliar to even my most seasoned RTs.
We had to come up with a new plan—quickly. We were being flooded with patients with COVID-19 at an alarming rate, and ventilator numbers were climbing. We had the idea to create a team whose only purpose was to go around the hospital to prone and supine patients. But where would we get the staff to create this team?
Building the “Prone Team”
Since surgeries and other services like physical therapy and occupational therapy were halted, we decided to pull operating room and interventional radiology nurses and technologists, along with physical therapists and occupational therapists, to create a multidisciplinary team. From this, the “Prone Team” was born.
 Members of Rush University Medical Center’s “Prone Team”
Members of Rush University Medical Center’s “Prone Team”
The Prone Team was led by an RT, and its members worked around the clock. With ventilator numbers eventually reaching almost 100 and with the majority of those patients requiring proning, the team came at the perfect time. Emotions and stress levels were running high, and the Prone Team helped relieve the bedside staff when they arrived to flip a patient.
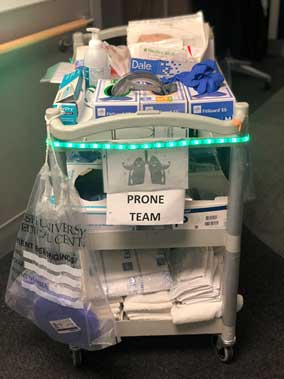 The “Prone Team” had a special cart of supplies to bring from patient to patient.
The team began to evolve and eventually came equipped with a cart of supplies decked out with LED lights and a speaker playing music. Everyone knew when the Prone Team was coming! The team remained in service for several months until the volume of prone patients returned to a more manageable state, and there finally was light at the end of the tunnel.
The “Prone Team” had a special cart of supplies to bring from patient to patient.
The team began to evolve and eventually came equipped with a cart of supplies decked out with LED lights and a speaker playing music. Everyone knew when the Prone Team was coming! The team remained in service for several months until the volume of prone patients returned to a more manageable state, and there finally was light at the end of the tunnel.
As a clinician, I will always remember being a part of implementing a new process during a global pandemic, as well as helping lead the Prone Team. It was an honor to witness colleagues from all disciplines come together and lend a helping hand for the betterment of our patients, and I am humbled to have led and formed a part of such an outstanding team of health care heroes.
 Tyler Weiss, MSc, RRT, RRT-ACCS, AE-C, is the Adult Clinical Education Coordinator and an Assistant Professor in the Department of Cardiopulmonary Sciences, Division of Respiratory Care, at Rush University Medical Center in Chicago.
Tyler Weiss, MSc, RRT, RRT-ACCS, AE-C, is the Adult Clinical Education Coordinator and an Assistant Professor in the Department of Cardiopulmonary Sciences, Division of Respiratory Care, at Rush University Medical Center in Chicago.
Read more COVID-19: Voices From the Community blog posts:
How APPs Helped Bridge the Staffing Gap During the COVID-19 Crisis
A Picture is Worth a Thousand Words
Medical Publishing in a COVID-19 World: How the Journal CHEST Adapted and Evolved